Online entertainment during the pandemic: comedy, quizzes, classes and more!
Click here for more information on staying mentally healthy at the moment.
In these worrying times it can be difficult to take our mind off the current situation, particularly without the opportunity to access usual entertainment, like popping into a museum or going to the cinema. However, in response to the pandemic many celebrities and creative minds have turned to the internet, to keep us entertained while we're stuck at home. If you know where to look, there is a huge amount of material online, from exercise videos, to live stand up and pub quizzes. Many are free, or raise money for charity. We have compiled a number of these here:
Dance lessons with Oti Mabuse and Marius Lepure
Stay fit and learn a new a new talent with these dance lessons from strictly professional Oti.
A weekly live-streamed comedy show. Every Saturday at 7pm. Tickets cost £2, with money going to the performers and The Trussell Trust.

If you're missing your local pub quiz, there are quizzes nearly every day of the week to be found. Every Thursday and Saturday, a general pub quiz is hosted live on YouTube from 8pm. On Fridays there is a guest host and there are shorter themed quizzes on other days. Watch live or find a backlog on YouTube. If you'd rather curate your own pub quiz to test friends and family at home or over Zoom, there have been a huge amount of questions posted online recently.
COVID-19 and Lung Disease
The European Lung Foundation has produced a useful Q and A session, to answer all of your questions about COVID-19 and existing lung conditions:
https://www.europeanlung.org/covid-19/covid-19-information-and-resources/covid-19-info
There is also a series of videos about COVID-19 in various patients produced by the European Respiratory Society - these are aimed at experts but may be interesting/of use to patients
https://dev.ers-education.org/covid-19/#webinar-series
Update June 23rd: UK government (via Cheshire CCG) guidance for patients in England who are shielding
The UK Government has set out a roadmap for the clinically extremely vulnerable on the future of the shielding programme.
For now, the guidance remains the same – stay at home and only go outside to exercise or to spend time outdoors with a member of your household, or with one other person from another household if you live alone – but the guidance will change on 6 July and again on 1 August, based on clinical evidence.
Shielding and other advice to the clinically extremely vulnerable has been and remains advisory.
What are the changes?
Recently, the UK Government advised that you can spend time outdoors, if you wish, with your own household, or if you live alone with another household. Following this, and alongside current scientific and medical advice, the UK Government is planning to relax shielding guidance in stages.
From 6 July, the guidance will change so you can meet in groups of up to six people from outside your household – outdoors with social distancing. For example, you might want to enjoy a summer BBQ outside at a friend’s house, but remember it is still important to maintain social distancing and you should not share items such as cups and plates. If you live alone (or are a lone adult with dependent children under 18), you will be able to form a support bubble with another household.
From 1 August, you will no longer need to shield, and the advice will be that you can visit shops and places of worship, but you should continue maintaining rigorous social distancing.
Why is the guidance changing now?
The roadmap has been developed in line with the latest scientific and medical advice and with the safety and welfare of those who are shielding in mind. Current statistics show that the rate of catching coronavirus in the community continues to decrease. On average less than 1 in 1,700 in our communities are estimated to have the virus, down from 1 in 500 four weeks ago.
Unless advised otherwise by your clinician, you are still in the ‘clinically extremely vulnerable’ category and should continue to follow the advice for that category, which can be found here.
We will monitor the virus continuously over coming months and if it spread too much, we may need to advise you to shield again.
If you are in receipt of Government provided food boxes and medicine deliveries, you will continue to receive this support until the end of July.
Local councils and volunteers are also providing support to people who are shielding, to enable them to stay safely in their homes. The government is funding local councils to continue to provide these services to those who need them until the end of July.
What support is available to people who are shielding until the end of July?
Essential supplies
There are a number of ways that those who are shielding can access food and other essentials:
- Make use of thesupermarket priority delivery slots that are available for this group. When a clinically extremely vulnerable person registers online as needing support with food, their data is shared with supermarkets. This means if they make an online order with a supermarket (as both a new or existing customer), they will be eligible for a priority slot.
- Use the many commercial options now available for accessing food, including telephone ordering, food box delivery, prepared meal delivery and other non-supermarket food delivery providers. A list has been shared with local authorities and charities.
- A free, standardised weekly parcel of food and household essentials. If you have registered for this support onlinebefore 17 July you will continue to receive weekly food box deliveries until the end of July.
- If you need urgent help and have no other means of support, contact your local council to find out what support services are available in their area.
- For anyone facing financial hardship, the government has made £63 million available to local councils in England to help those who are struggling to afford food and other essentials.
NHS Volunteer Responders
Support will continue to be available through the NHS Volunteer Responder Scheme beyond the end of July.
NHS Volunteer Responders can support you with:
- Collecting shopping, medication (if your friends and family cannot collect them for you) or other essential supplies;
- A regular, friendly phone call which can be provided by different volunteers each time or by someone who is also shielding and will stay in contact for several weeks; and
- Transport to medical appointment.
Please call 0808 196 3646 between 8am and 8pm to arrange support or speak to your health case professional for transport support. A carer or family member can also do this on their behalf. More information is available at www.nhsvolunteerresponders.org.uk
Health care
Any essential carers or visitors who support you with your everyday needs can continue to visit unless they have any of the symptoms of COVID-19 (a new continuous cough, a high temperature, or a loss of, or change in, their normal sense of taste or smell).
People in the clinically extremely vulnerable group should continue to access the NHS services they need during this time. This may be delivered in a different way or in a different place than they are used to, for example via an online consultation, but if they do need to go to hospital or attend another health facility for planned care, extra planning and protection will be put in place.
Mental health support
It is normal during these uncertain and unusual times to feel anxious or feel low.
Follow the advice that works for you in the guidance on how to look after your mental health and wellbeing during coronavirus (COVID-19).
The Every Mind Matters page on anxiety and NHS mental wellbeing audio guides provide further information on how to manage anxiety.
If you feel you need to talk to someone about your mental health or you are looking for more support for someone else, we would urge you to speak to a GP and seek out mental health support delivered by charities or the NHS.
Income and employment support
At this time, people who are shielding are advised not to go to work. This guidance remains advisory.
Those shielding will be eligible for Statutory Sick Pay (SSP) on the basis of their shielding status until the 31 July. SSP eligibility criteria apply
From 1 August, if clinically extremely vulnerable people are unable to work from home but need to work, they can, as long as the business is COVID safe.
The Government is asking employers to work with them to ease the transition back to a more normal way of life for their shielding employees. It is important that this group continues to take careful precautions, and employers should do all they can to enable them to work from home where this is possible, including moving them to another role if required.
Where this is not possible, those who have been shielding should be provided with the safest onsite roles that enable them to maintain social distancing.
If employers cannot provide a safe working environment, they can continue to use the Job Retention Scheme for shielded employees who have already been furloughed.
What support will be available after July?
From 1 August, clinically extremely vulnerable people will continue to have access to priority supermarket delivery slots if you have registered online before 17 July for a priority delivery slot.
NHS Volunteer Responders will also continue to offer support to those who need it, including collecting and delivering food and medicines.
The NHS Volunteer Responders Scheme has been expanded to offer a new Check in and Chat Plus role. This new role has been designed to provide peer support and companionship to people who are shielding as they adapt to a more normal way of life.
If you are vulnerable or at risk and need help with shopping, medication or other essential supplies, please call 0808 196 3646 (8am to 8pm).
Government is committed to supporting local councils and voluntary sector organisations to respond to those who have specific support needs and requirements during the COVID-19 pandemic. Details of the support and advice available can be found here: https://www.gov.uk/find-coronavirus-support
The updated shielding guidance should not affect any social care or support you were receiving prior to the start of shielding.
Individuals should continue to contact their local council if they have any ongoing social care needs.
Fungal spore and air quality forecasts
[et_pb_section fb_built="1" admin_label="section" _builder_version="4.16" global_colors_info="{}" theme_builder_area="post_content" custom_padding="3px||3px||true|false"][et_pb_row admin_label="row" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.16" custom_padding="|||" global_colors_info="{}" custom_padding__hover="|||" theme_builder_area="post_content"][et_pb_text admin_label="Text" _builder_version="4.21.0" background_size="initial" background_position="top_left" background_repeat="repeat" hover_enabled="0" global_colors_info="{}" theme_builder_area="post_content" sticky_enabled="0"]
Good air quality is important for everyone's health. However, those with lung conditions, such as aspergillosis and asthma, may be more vulnerable to the effects of poor air than others. Airborne pollutants and allergens are found both indoors and outdoors, and can irritate our lungs and exacerbate existing conditions. It can be useful, therefore, to know when and where these irritants are at their most harmful concentrations — this can allow us to understand, avoid and prevent any harmful air conditions that may be affecting our health. Here we have compiled a selection of air quality forecasts and information:
Fungal Spores
Fungal spores are microscopic particles responsible for the reproduction of fungi. We inhale huge numbers of these particles in each breath — for most people, this doesn't affect their health. However, some individuals, including aspergillosis patients, are more susceptible to allergic reactions and infections from mould spores. It can therefore be useful to know when mould spores are at their highest concentrations, in order to reduce exposure to them. We are currently entering peak spore season for most moulds (June - August). Peak spore season coincides with hayfever season, and allergies to pollen and spores carry similar symptoms (runny nose, sore eyes, rashes). Therefore, it is often difficult to distinguish between these conditions, and medical tests may be necessary.
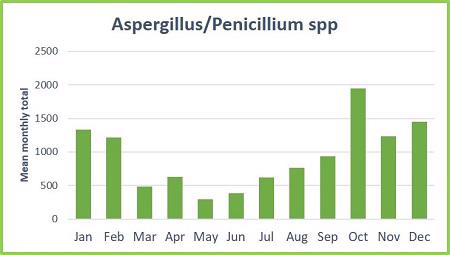
The National Pollen and Aerobiology Research Unit at the University of Worcester has produced a number of helpful calendars, showing the monthly spore count averages over a period of 5 years. They have also compiled useful information on the allergenicity of each spore type and where each mould prefers to grow. This allows those at risk to avoid areas where the spore concentration is potentially very high. The information for Aspergillus/Penicillium spp. is copied below:
The year starts with a high risk for these types with a total monthly average of 1,333 (per m3) spores in January and 1,215 in February. Spores continue to be airborne during Spring and early Summer but possibly below the levels needed to trigger symptoms. From mid-August the risk starts to rise again and people often report symptoms during warm, humid conditions in late August, September and October, with the peak reaching an average of 1,950 spores in October. Although the spore levels continue to be high during November and December, few people report symptoms, so it is likely that the types occurring during these months are less allergenic.
Habitat / Substrates:
There are many species of Aspergillus and Penicillium, which live on a wide range of substrates. The spores can be very prevalent during the peak periods, triggering a range of respiratory problems. The spores are particularly prevalent in wooded areas, compost heaps, rotting wood chips and bark mulch. Some species rot down pine needles, so conifer plantations should be avoided during Autumn. Penicillium chrysogenum is found widely in nature, occurs on indoor substrates and is the type used to produce the antibiotic penicillin. N.B. Houseplants can be sources of spores, particularly Aspergillus/Penicillium types. If you’re keen to have houseplants, only have cacti, which require dry conditions, and ensure the soil surface is covered in grit.
Season:
Aspergillus and Penicillium spores are present in the air throughout the year but the main peak periods are late August to October and January to February.
Allergenicity:
High for some types, particularly A. fumigatus and P. chrysogenum. A. fumigatus is a major cause of aspergillosis (farmer’s lung).
For spore forecasts and information about other species:
For regular updates on pollen and spore counts:
- The Midlands Asthma and Allergy Research Association (UK)
- National Pollen and Aerobiology Research Unit (UK)
- The Asthma Center (US)
Indoor air
Those self-isolating due to COVID-19 are spending almost all of their time at home. Therefore, indoor air quality is more of a concern than ever. Over the past ~50 years, our homes have become far more insulated. While this stops drafts and keeps our homes warmer, it also means than our living spaces are generally damper and less ventilated. This can provide ideal conditions for mould to grow and thrive. There are a number of small things that we can do to prevent mould and damp: these include drying laundry outside (if possible), fixing leaks and using lids when cooking. It is also important to identify and remove any mould in your living space, in order to prevent it from spreading. A selection of articles on indoor air quality and instructions for how to safely remove mould are listed below.
For more information:
- Damp homes
- Indoor air pollution
- Dehumidifiers
- Air conditioning units
- Anti-allergen products
- How do I… find the source of the damp?
- How do I… remove mould from my washing machine?
- How do I… make my private landlord fix my damp home?
- How do I… make the council fix my damp home?
- How do I… keep my home dry?
Pollution
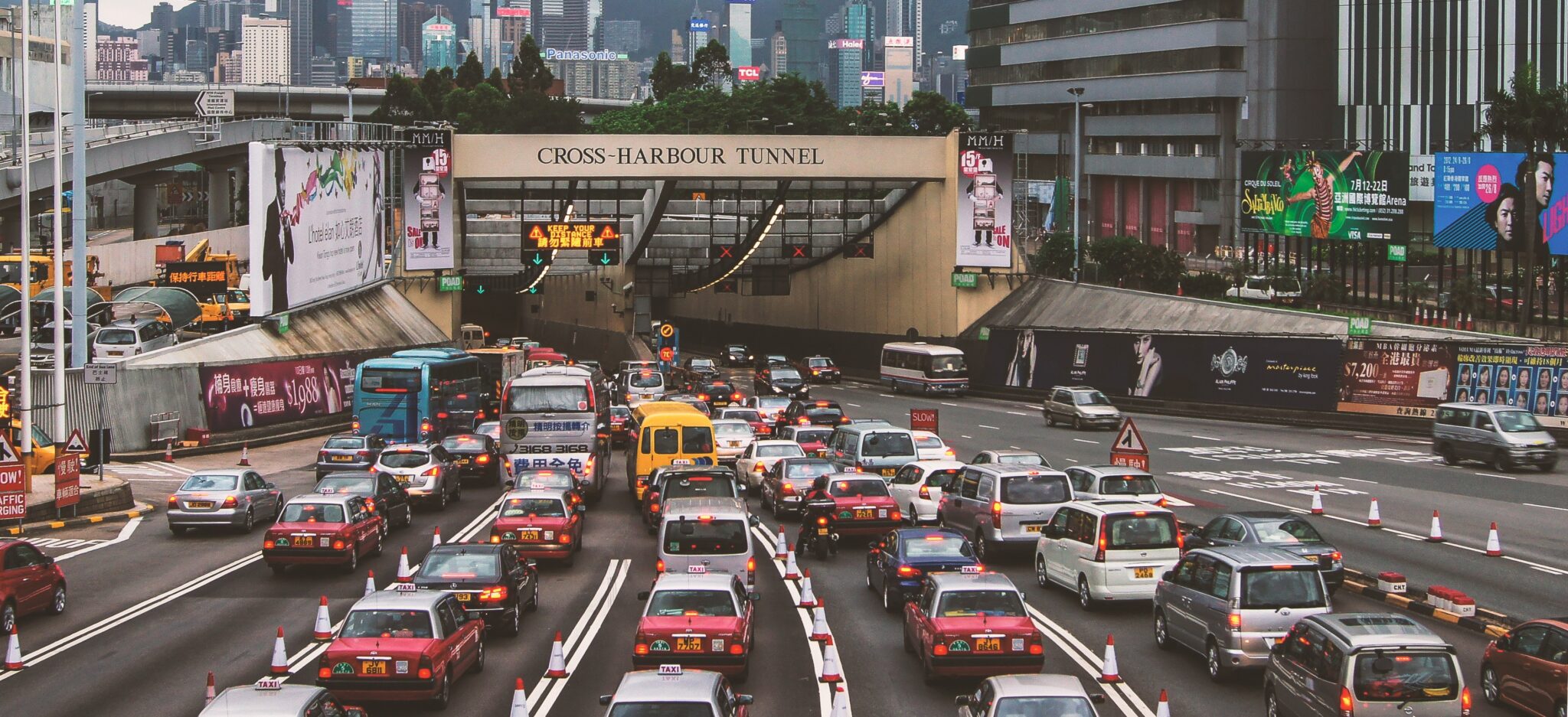
Air pollution is a significant health concern, especially for those living with existing lung conditions. This is a particular issue in urban areas, where the sources of pollutants are concentrated. Weather also influences levels of pollution, with stiller conditions often worsening the issue. It can therefore be useful to access pollution forecasts, so that high levels can be avoided, where possible.
Regularly-updated pollution forecasts for the UK and worldwide:
For further information on air quality:
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Living with hyper-IgE syndrome and aspergillosis: patient video
[et_pb_section fb_built="1" admin_label="section" _builder_version="4.16" global_colors_info="{}" theme_builder_area="post_content"][et_pb_row admin_label="row" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.16" custom_padding="|||" global_colors_info="{}" custom_padding__hover="|||" theme_builder_area="post_content"][et_pb_video src="https://breathe.ersjournals.com/content/breathe/15/4/e131/DC1/embed/inline-supplementary-material-1.mp4?download=true" _builder_version="4.19.1" _module_preset="default" hover_enabled="0" global_colors_info="{}" theme_builder_area="post_content" sticky_enabled="0"][/et_pb_video][et_pb_text admin_label="Text" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content"]
The following content is reproduced from ERS Breathe Vol 15 Issue 4. Click here to view the original article.
In the above video, Sandra Hicks summarises her experience with hyper-IgE syndrome (HIES), a primary immunodeficiency syndrome, and how living with this rare genetic condition and associated lung infections impacts her life. As a direct consequence of HIES and its effect on the immune cascade, Sandra concurrently manages chronic Aspergillus infection (aspergillosis), nontuberculous mycobacterial infection (Mycobacterium avium-intracellulare), bronchiectasis colonised with Pseudomonas and asthma. She discusses the effect this rare disease and infection burden have on her daily life, including the influence of other factors such as temperature, humidity and antimicrobial resistance.
Sandra conveys her hopes for clinicians treating others with similar disease profiles, including the impact of immunoglobulin treatment; early, accurate diagnosis of primary immunodeficiencies and fungal infections; and awareness of potential interactions between antifungals and other medication (https://antifungalinteractions.org). She also discusses the importance of comprehensive, timely communication within and between multidisciplinary teams. Finally, Sandra emphasises the value of support from allied healthcare professionals for people with chronic lung conditions.
Sandra has since returned to pulmonary rehabilitation classes. These provide great benefit, not just for people with COPD but also for those living with other lung conditions. Making this service widely accessible would improve management of chronic lung conditions and could even reduce associated healthcare costs.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
The New York Times on the dangers of mould
Those living with aspergillosis know all too well the risks associated with mould exposure. It can be difficult, however, to sort fact from horror story on the internet sometimes. Damp and mould in the home can be a serious issue, both for those with and without pre-existing illnesses — it is therefore very important to understand the risks and take measures to identify and prevent any sources of mould growth. The New York Times has written a very useful article, quoting Professor David Denning of the National Aspergillosis Centre, on the known health consequences of mouldy homes and the importance, and difficulty, of removing the fungus.
Read the article here:
Mold Can Make Your Family Sick. Here’s How to Get Rid of It.

For more advice:
- How do I… find the source of the damp?
- How do I… remove mould from my washing machine?
- How do I… make my private landlord fix my damp home?
- How do I… make the council fix my damp home?
- How do I… keep my home dry?
Extraordinary images of Aspergillus restrictus
[et_pb_section fb_built="1" admin_label="section" _builder_version="4.16" global_colors_info="{}" theme_builder_area="post_content" custom_padding="12px||12px||true|false"][et_pb_row admin_label="row" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.16" custom_padding="|||" global_colors_info="{}" custom_padding__hover="|||" theme_builder_area="post_content"][et_pb_text admin_label="Text" _builder_version="4.21.0" background_size="initial" background_position="top_left" background_repeat="repeat" hover_enabled="0" global_colors_info="{}" theme_builder_area="post_content" sticky_enabled="0"]
In 2017, the Dutch Central Bureau of Fungal Cultures was renamed the Westerdijk Fungal Biodiversity Institute, after Johanna Westerdijk. Westerdijk was the first female professor of The Netherlands and director of the centre from 1907 to 1952. She had a great interest in fungi and, under her leadership, the institute's collection grew to be the largest in the world. A century on from her appointment as professor, Westerdijk's accomplishments were celebrated with the centre's renaming and the unveiling of several extraordinary images of Aspergillus restrictus.
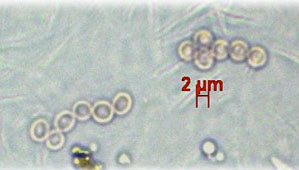
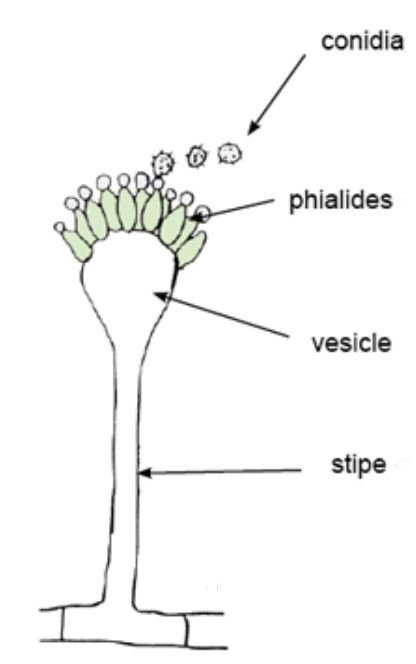
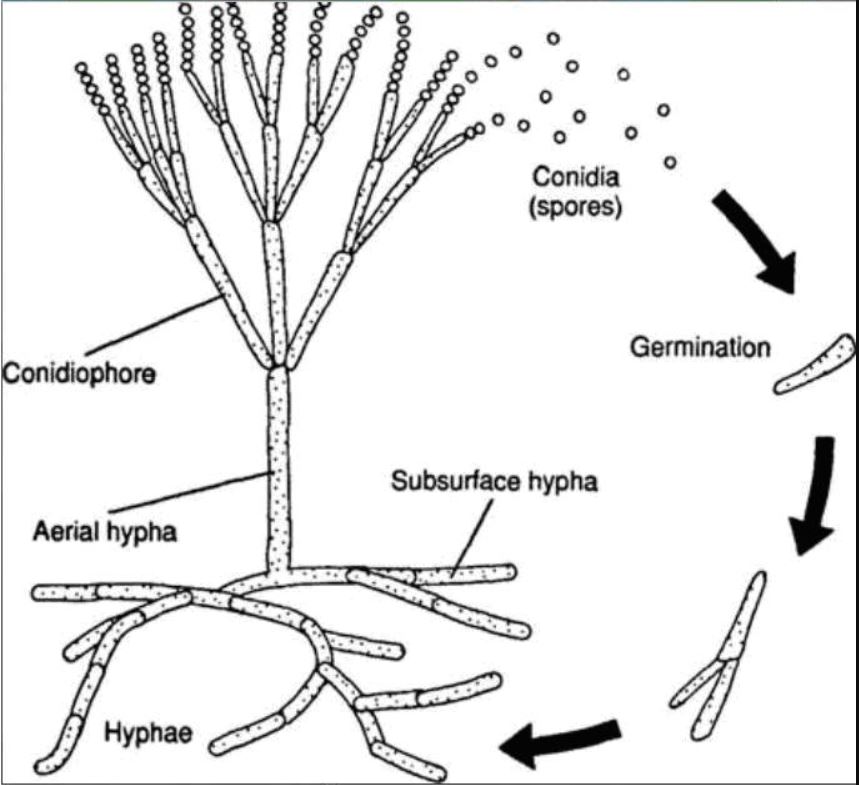
A. restrictus is a mould that can grow in environments with very limited water. The species is often found in indoor air and house dust, and is considered a potential cause of respiratory issues; A. restrictus can also contribute towards cereal and cotton rot. In this project, high resolution images of the species were taken at various magnifications, using both light and electron microscopy. These images, copied below, allow the viewer to zoom in on the structure of the mould at differing levels of detail. This means that we can explore the various stages of fungal growth, from different angles and magnifications. For reference, simplified diagrams of the Aspergillus life cycle and structure are included first.
Images of Aspergillus restrictus:

An Aspergillus restrictus colony, measuring approximately 1 cm (bar = 1 mm). White aerial hyphae can be seen throughout the colony.[/caption]
 An image taken closer to the centre of the colony (bar = 0.5 mm). White aerial hyphae and green columnar conidiophores can be seen throughout.
An image taken closer to the centre of the colony (bar = 0.5 mm). White aerial hyphae and green columnar conidiophores can be seen throughout.
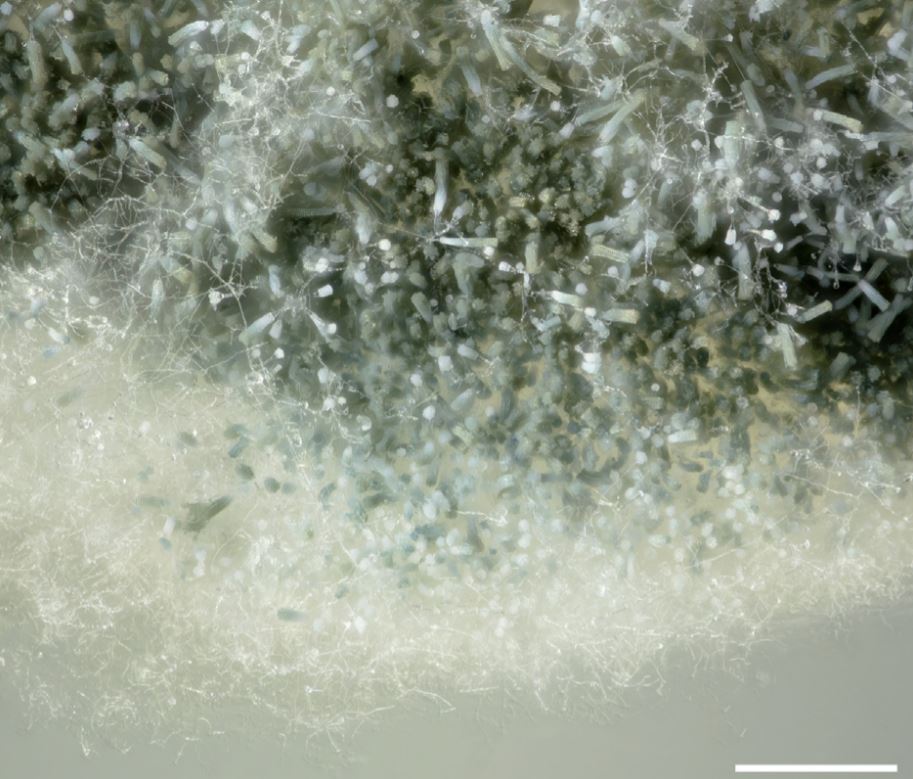
These images, produced by the Westerdijk Fungal Biodiversity Institute, show the structure and development of Aspergillus restrictus in incredible detail. There are several surprising questions and discoveries that arise from this level of detail. For example, the clockwise twisting of conidial rows has not previously been described, and the chemical composition of the material found on the phialide surfaces is unknown. Therefore, this technology not only provides us with these impressive images, but may also lead to further research and greater understanding of the structure and development of fungi. Greater knowledge of Aspergillus growth and function can assist in the development of drugs which impede its growth.
Read the full paper: Jan Dijksterhuis, Wim van Egmond and Andrew Yarwood (2020), From colony to rodlet: “A six meter long portrait of the xerophilic fungus Aspergillus restrictus decorates the hall of the Westerdijk institute.”
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
May 31st: Shielding Advice Updated by Public Health England
Many people with Chronic Pulmonary Aspergillosis were asked to shield themselves from exposure to the coronavirus COVID-19 in March 2020 as they were thought to be especially vulnerable to the consequences of infection by the respiratory virus.
Back in March 2020 the COVID-19 pandemic was progressing rapidly and there was some doubt about how well we might be able to contain it in the UK using a variety of social spacing measures, consequently, it was appropriate for the most vulnerable to be especially protected. We also knew relatively little about the virus and how it is transmitted, which groups might be more vulnerable to infection and severe symptoms.
More recently, by late May 2020 the pandemic in the UK is currently well under control with the number of cases in the community falling rapidly week on week, estimated at 17% between May 10 and 21st (AskZoe).
There is a real risk that extending shielding will have an overall detrimental impact on health, particularly on the mental health of those shielding, so it is important that we limit the numbers of people to those who absolutely have to, and ease up restrictions on those that have to carry on when it is deemed safe enough to do so.
The overall authority in England is Public Health England (PHE) and they released updated guidelines for people who are shielding here on 31st May 2020.
What has changed
The government has updated its guidance for people who are shielding taking into account that COVID-19 disease levels are substantially lower now than when shielding was first introduced.
People who are shielding remain vulnerable and should continue to take precautions but can now leave their home if they wish, as long as they are able to maintain strict social distancing. If you choose to spend time outdoors, this can be with members of your own household. If you live alone, you can spend time outdoors with one person from another household. Ideally, this should be the same person each time. If you do go out, you should take extra care to minimise contact with others by keeping 2 metres apart. This guidance will be kept under regular review.
Read further information on schools and the workplace for those living in households where people are shielding. This guidance remains advisory.
Advice for Wales (updated but there may be some differences to PHE advice)
Advice for Scotland (not yet changed so are now different to England & Wales)
Advice for Northern Ireland (not yet changed but may change on June 8th)
Can I have ABPA without asthma?
[et_pb_section admin_label="section"]
[et_pb_row admin_label="row"]
[et_pb_column type="4_4"][et_pb_text admin_label="Text"]Allergic bronchopulmonary aspergillosis (ABPA) generally occurs in patients with asthma or cystic fibrosis. Little is known about ABPA in patients without asthma — entitled "ABPA sans asthma" — despite it having first been described in the 1980s. A recent study, performed by Dr Valliappan Muthu and colleagues at the Postgraduate Institute of Medical Education and Research, Chandigarh, India, has looked at the records of ABPA patients with and without asthma, in order to find clinical differences between the two disease subsets.

The study included 530 patients, with 7% of those identified as having ABPA sans asthma. This is the largest known investigation of the disease to date. However, as the research was conducted retrospectively at a specialist centre, and ABPA sans asthma is a difficult condition to diagnose, the true number of those affected is unknown.
Certain similarities were found between the two disease types. There were similar rates of coughing up blood (haemoptysis) and coughing up mucus plugs. Bronchiectasis, a condition where the airways are widened and inflamed, was found more often in those without asthma (97.3% vs 83.2%). However, the extent to which the lung was affected by bronchiectasis was similar in both groups.
Lung function tests (spirometry) were significantly better in those without asthma: normal spirometry was found in 53.1% of those without asthma, in comparison to 27.7% of those with asthma. Furthermore, ABPA sans asthma patients were significantly less likely to experience ABPA exacerbations.
To sum up, this study found that those experiencing ABPA sans asthma were likely to have better lung function and fewer exacerbations than those with ABPA and asthma. However, clinical symptoms, such as mucus pugs and haemoptysis occurred at similar rates and bronchiectasis was more common in ABPA sans asthma patients. This was the largest study to date on this subset of ABPA; however, further research is required to understand the condition better.
Full paper: Muthu et al. (2019), Allergic bronchopulmonary aspergillosis (ABPA) sans asthma: A distinct subset of ABPA with a lesser risk of exacerbation[/et_pb_text][/et_pb_column]
[/et_pb_row]
[/et_pb_section]
Living with a lung condition during the COVID-19 pandemic: patient stories
The current pandemic is a frightening time for us all, but it can be especially nerve-wracking for those already living with lung conditions. The European Lung Foundation has compiled 4 stories from individuals living with pre-existing lung diseases, and their experiences living through this period. One contribution is from an aspergillosis patient and co-founder of the Aspergillosis Trust, Sandra Hicks, and has been copied below. To read all of the contributions, or share your own experience, click here.
The Aspergillosis Trust has also continued to collect and share the experiences of those living with aspergillosis during this time. To read and share stories, or find out more about the Trust's work, click here to visit their website.
Sandra Hicks:
During the last weekend of February 2020, I had a bit more of a productive cough than usual. I stayed in bed, as I felt even more fatigued than usual and that’s already a lot! I have aspergillosis, Nontuberculous Mycobacteria (NTM), asthma and bronchiectasis colonised with Pseudomonas. The reason for these unusual infections is a rare primary immunodeficiency (PID) syndrome, which means that my immune system doesn’t make antibodies very well.
On 1 March, I had a severe pain in my right side, it felt to me like I had pulled a muscle between my ribs and another in my neck. The pain was so bad that I could hardly cough and I certainly couldn’t breathe in deeply. I also had worsening shortness of breath. I realised it was better to get on top of the pain, to be able to clear my lungs. I had a productive cough, not a persistent, dry cough as listed in the COVID-19 symptoms. I felt it didn’t really match with the description of the ‘red flags’ for COVID-19. I didn’t have a sore throat at any point. I did have a high temperature, which went up to 39.5°C during the first week of March. I also had headaches and dizziness, but didn’t lose my sense of taste or smell. The final symptom was coughing-up dark red, thick mucous (haemoptysis) a few times a day, for several weeks. I have never had haemoptysis to that extent ever before, or that dark a red (although the mucous can sometimes be ‘pinky’ in colour).
My routine CT scan which I have for the aspergillosis showed improvements and did not reflect the development of haemoptysis. So it seemed to me like something else was going on in addition to the usual lung problems.
I had phone consultations instead of outpatient clinic appointments with two consultants. The first one was with my mycology consultant on 25 March. He felt that it was possible that I could have had COVID-19. We discussed options for my regular treatment. Should I go into hospital daily for my 14 days of IV caspofungin, or should I delay treatment? Even if I hadn’t had COVID-19, I am in the shielding category and had been advised to stay at home for 12 weeks. The balance of risks were in favour of starting treatment sooner. This was due to the lower numbers of cases of COVID-19 in the UK at that time, compared to the rest of Europe. I was concerned that if we followed the same pattern as Italy, Spain and France, then in the next 2-3 weeks, the number of cases and deaths would rise hugely. When that cycle of treatment started on 30 March, there were 1,408 deaths from COVID-19 reported in the UK. On Easter Sunday, 12April the last day of treatment, there were 10,612 deaths reported in the UK. It was a very scary time, having to go into hospital daily during those two weeks. If I had delayed treatment, the hospital might not have had capacity to treat me. My lung condition could also have deteriorated. I may have been at greater risk of catching COVID-19 too. Looking back, it turned out to be the right decision for me.
My immunology consultant also said on 27 March in another phone appointment, that it was possible I’d had COVID-19. However, there is no way of knowing for sure if I have. COVID-19 blood tests look for the presence of antibodies produced by the immune system. If these antibodies are present, then that means a person has had the infection in the past. However, these tests might not be accurate in people with primary immunodeficiency syndromes, because we don’t always make antibodies properly. The consultant said that they do not yet know for sure whether having COVID-19 means that you will develop immunity. He also said that if patients need to come in for procedures then they take measures to prevent infection: they pull the curtains in between beds, everyone wears masks, staff also wear aprons and gloves.
So, I still don’t know if I have had COVID-19, but it is possible! I will probably never know either. If this was mild or moderate COVID-19, it was still bad enough on top of the usual lung conditions.
It is an incredibly sad situation that so many people have lost their lives prematurely. The current total number of deaths in the UK is 34, 636 (18 may). It’s so important to stay at home for those of us with lung disease, who are most at risk. I personally don’t see a ‘quick fix’ for this pandemic and it is possible there will be a second and third wave. I am looking forward to the vaccine being available, so it protects more people.