We Are Undefeatable
We Are Undefeatable is a campaign which aims to help those with chronic health conditions exercise. Both the conditions and forms of exercise vary widely - the goal is to find out what works best for you!
Visit the website to discover how exercise has helped other people with chronic conditions, and what the campaign can do for you : We Are Undefeatable
For more information on exercises specific to aspergillosis and chronic lung conditions:
- How do I exercise in a bed or chair?
- Your lungs and exercise
- BLF: Keeping active with a lung condition
Aspirin may reduce harmful effects of air pollution on lungs

A recent study by Dr Xu Gao and colleagues has looked at the relationship between lung function and the use of non-steroidal anti-inflammatory drugs (which include aspirin) in 2,280 veterans. The researchers then compared this with air pollution data from the previous month in their hometown of greater Boston. Other factors, including whether or not the participant was a smoker were also taken into consideration.
The study found that NSAIDs nearly halved the effect of particulate matter (all solid and liquid particles suspended in air) on lung function. The mechanism by which this protection happens is unknown, but may be due to NSAIDS reducing inflammation in the lung caused by pollution. As most of the participants in the study were taking aspirin, this effect was deemed to be predominantly due to aspirin, but the effect of other NSAIDs would be useful to study.
These results show that aspirin may be useful in the short-term protection of lungs against air pollution. However, air pollution contributes to a number of other harmful bodily effects so it is still important to minimise overall exposure.
To check air pollution in your area, click here
References:
- Aspirin may halve air pollution harms
- Nonsteroidal Anti-Inflammatory Drugs Modify the Effect of Short-Term Air Pollution on Lung Function
Fungal biofilm structure and its indications in invasive aspergillosis

Microorganisms can group together on a surface to form collections of cells called biofilms; one example of this is dental plaque. Grouping together as a community protects these cells from environments which they may not be able to survive alone, such as the wrong pH or a lack of water or oxygen. Biofilms may be made up of many different species of microorganism and these species may be varied further by strain. In a recent paper, Caitlin Kowalski and colleagues at the Geisel School of Medicine at Dartmouth, USA, studied the ability of Aspergillus fumigatus biofilms to grow in low oxygen environments and cause invasive aspergillosis in mice.
Kowalski and colleagues exposed A. fumigatus to low levels of oxygen, which reflect the levels found in the lesions where the fungus grows in the lung, in order to identify genes and mechanisms involved in allowing the pathogen to grow under these conditions. They then discovered a specific mutation which allowed the strain to both grow better in low oxygen, but also cause disease better under these conditions. It remains to be discovered how this particular mutation allows the strain to grow more successfully and be more virulent in low oxygen. However in other fungal biofilms, for example the yeast Candida albicans, the colony can form wrinkles which improve oxygen penetration. Understanding how the structure of biofilm colony growth reflects advantages in the ability of the fungus to cause disease may allow clinicians and scientists to better predict the progression of disease and improve patient care.
Find out more:
- Fungal biofilm morphology impacts hypoxia fitness and disease progression.
- How fungal biofilm structure impacts lung disease
“Aspergillus and me” by Los Trensplantados
“Aspergillus and me” is a song written by Alessandro Pasqualotto, a medical mycologist from Brazil, and two transplant patients, Jimi Joe (kidney), and King Jim (liver).
The initiative started when King was hospitalized due to a chronic cough. King is known for being asthmatic and he has some mild bronchiectasis, in addition to being a liver transplant recipient. A bronchoalveolar lavage (BAL) was performed, and Pseudomonas aeruginosa was recovered in culture, in addition to Aspergillus fumigatus (galactomannan testing was not performed). At that time, Alessandro Pasqualotto visited King in the hospital primarily as a fan, not as a physician. After collecting several autographs in vinyl albums from the 80’s (King was part of the famous rock band Garotos da Rua), Pasqualotto and King started a discussion on the relevance of A. fumigatus in his BAL exam. Despite being treated with voriconazole by order of the medical team in charge, Pasqualotto thought the musician was only colonized by the fungus. The dilemma surrounding the relevance of Aspergillus in this context motivated both Pasqualotto and King to write a song about that.
After being discharged from the hospital, King collected a group of experienced musicians to record Pasqualotto’s song. This included Jimi Joe, a kidney transplant recipient who together with King formed the band “Los Tresplantados”, a group of three transplant musicians that approaches the importance of organ donation, as well as opportunistic infections. Los Tresplantados, however, have never written a song about fungal infections, so this was a great opportunity to increase people’s awareness of such important diseases.
So this is what “Aspergillus and me” are all about. Alternatively, musicians also refer to this song as “When Black Sabbath meets Neil Young”. We hope you enjoy the song!
Contacts: Alessandro C. Pasqualotto (acpasqualotto@gmail.com)
WhatsUp number: +55 51 999951614
Interview link (Portuguese only): https://www.youtube.com/watch?v=ZyywH0LtS50
Sunflower lanyards: support for travelling with invisible illnesses

Travelling through airports with an invisible illness can be difficult, as it may not be obvious to others that you need extra time or assistance. The experience can be stressful and anxious for some, and it may be hard to explain your hidden symptoms. This is why several airports in the UK have implemented a scheme, so that those with invisible illnesses can order a sunflower lanyard to wear through the airport. These lanyards make the wearer more visible so that they can travel independently, but access help quickly if needed. Some supermarkets are also trialing this scheme.
To find out more about sunflower lanyards, click here
Side effects of long-term azole therapy
Azole antifungals are the first-line of treatment or prophylaxis for many fungal infections. They are often administered long-term (weeks to months), which can be associated with a number of adverse effects. In patients receiving several medications, it can be difficult to identify whether antifungals are contributing to, or causing particular symptoms; recognition of common side effects, leading to treatment discontinuation or management, is therefore key to reducing symptoms and reversing toxicity. A recent review by Dr Lydia Benitez and Dr Peggy Carver summarises these effects and their frequency:
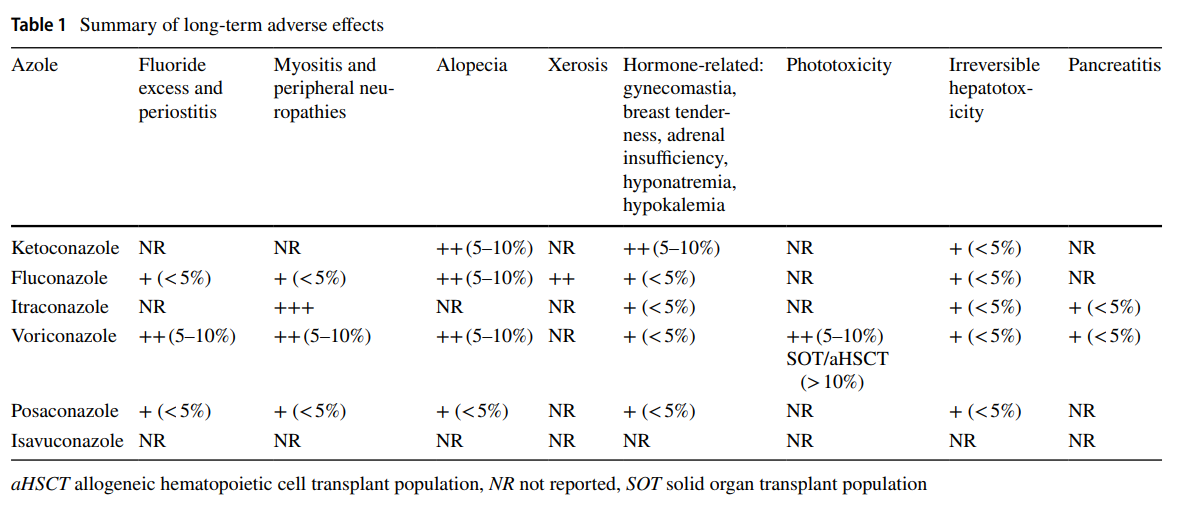
Key points the authors highlight:
- Liver toxicity, generally reversible, is common with all azoles.
- Hormone-related adverse effects are observed with select azoles; these include hair loss, breast enlargement, decreased libido, impotence, and (rarely) adrenal insufficiency (beware drug interactions with inhaled and oral steroids).
- Patients with fair skin on voriconazole should use liberal amounts of broad spectrum UV protectants and wear sun protective clothing, avoid excess sunlight, and undergo frequent monitoring of skin as phototoxic reactions progressing to development of skin cancer has been associated with long-term use.
- Therapeutic drug monitoring may be utilized to minimise neuropathies in specific patient populations on voriconazole, as neuropathies are more common with higher concentrations and doses. Its role in preventing other long-term toxicities is less clear.
Azoles are a valuable resource in the treatment and prophylaxis for fungal infections. Despite being associated with a number of adverse effects, they are safer and more active than alternatives. Thorough knowledge of the side effects they may cause is therefore important, so that they can be recognised and managed promptly.
Read the paper here: Benitez, L.L. & Carver, P.L. Drugs (2019) 79: 833
Vitamin D deficiency may increase the risk of Amphotericin B-related kidney toxicity

Amphotericin B (AmB) is the drug of choice for the treatment
of many fungal infections. Despite this,
the drug can cause several serious side effects, one of which being nephrotoxicity
(toxicity to the kidneys). Conventional AmB can be adapted into a lipid
emulsion preparation, which can reduce the risk of nephrotoxicity, while
preserving its efficacy and remaining a lower cost option. Unfortunately this
does not solve the problem, and nephrotoxicity remains an issue for many
patients.
Vitamin D deficiency has been found to be a major problem worldwide, and can increase the risk of kidney-related disease, including drug-induced nephrotoxicity. A recent study by Daniela Ferreira and colleagues at the University of Sao Paulo looked at standard and vitamin D-deficient rats and found that the deficient rats treated with AmB presented with impaired renal function. This suggests that vitamin D deficiency may play a key role in the development of AmB-induced nephrotoxicity. Therefore, the authors state that it is essential to monitor levels of vitamin D in patients treated with both conventional and lipid formulations of AmB, in order to reduce the development of kidney disease.
New diagnostic tool paves the way for faster and earlier diagnosis of chronic pulmonary aspergillosis

A new screening test kit will speed up diagnosis of chronic pulmonary aspergillosis (CPA) say researchers from the University of Manchester. The test, available commercially from LDBio diagnostics, is very simple and needs no power source or equipment and therefore is likely to be very useful in resource poor settings.
CPA is a fungal disease associated with lung damage caused by other conditions including TB which is prevalent in low to middle income countries. CPA can get progressively worse over time and so early diagnosis is crucial to improve patient outcomes.
The team from the University of Manchester and the NHS Mycology Reference Centre, based at Wythenshawe Hospital, tested the LDBio Aspergillus ICT kit on blood samples collected from 154 CPA patients identified at the National Aspergillosis Centre in Manchester and 150 healthy volunteers. They found that the test had improved sensitivity (91.6%) and specificity (98.0%) for diagnosis of CPA in UK patients compared to existing diagnostic tests.
Limitations of current diagnostic procedures include high cost, long turn-around times, poor reproducibility and variations in performance. The new test is cheap, fast, reproducible and reliable. Therefore it is particularly useful in low to middle income countries where CPA diagnostics are a necessity for early recognition of CPA complicating TB, and to distinguish between these similarly presenting conditions.
Professor David Denning, Professor of Infectious Diseases in Global Health at the University of Manchester and Director of the National Aspergillosis Centre at the Manchester University NHS Foundation Trust said:
"With over 7 million people suffering TB in the lungs each year and 5-10% of them later getting the fungal infection aspergillosis in the lungs, a simple cost-effective test for aspergillosis is sorely needed. This new test fulfils these basic requirements and we are delighted to report that its diagnostic performance surpasses all the older tests as well. A real win-win for early diagnosis and reducing lung scarring and death."
The findings were published this month in the Journal of Clinical Microbiology.
Citation:
Evaluation of LD Bio Aspergillus ICT lateral flow assay for IgG and IgM antibody detection in chronic pulmonary aspergillosis. Elizabeth Stucky Hunter, Malcolm D. Richardson, David W. Denning. Journal of Clinical Microbiology Jun 2019, JCM.00538-19; DOI: 10.1128/JCM.00538-19
Positive expiratory pressure (PEP) therapy
[et_pb_section fb_built="1" admin_label="section" _builder_version="4.19.1" hover_enabled="0" global_colors_info="{}" theme_builder_area="post_content" sticky_enabled="0"][et_pb_row admin_label="row" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content" custom_margin="11px|auto|11px|auto|true|false" custom_padding="0px|23px|0px|0px|false|false"][et_pb_column type="4_4" _builder_version="4.16" custom_padding="|||" global_colors_info="{}" custom_padding__hover="|||" theme_builder_area="post_content"][et_pb_text admin_label="Text" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content" custom_margin="|-23px||||"]
The aim of physiotherapy for chest clearance is to remove the excess secretions which are produced by the lungs in response to infection, virus or toxins from fungal stimulus. Regular maintenance treatment is important to keep a clear chest and reduce the need for repeated courses of antibiotics.
Three Aims of Chest Clearance are to optimise the muco-cilary escalator, maintain open airways reducing wheeze, and generate air flow in the airways, getting air behind the phlegm to help push it upwards from the small airways towards the mouth. The aim of physiotherapy is to do all of these things in the most energy and time efficient way possible. This is not as complicated sounds and your physiotherapist will help you build a personalised plan to work best with your lungs, an example of a maintenance chest physiotherapy treatment plan is shown below.
- Optimise the mucocilary escalator: Hypertonic Saline(See below), increase oral hydration and fluid intake.
- Maintain open airways to allow the upward movement sputum: Bronchodilators / inhalers will help relax and open the small airways and reduce wheeze, and the Pari O-PEP will splint them open also as you blow out through the PEP device.
- Generate air flow in the airways: Deep breathing exercises gets air in behind the sputum to push if from lower in the airways to higher up in the chest, oscillations from the OPEP device helps by adding to turbulence in airways.
Example Patient’s Physiotherapy Treatment Plan |
|
Seretide 250 Evohaler Inhaled Bronchodilator therapies help to open up and relax the airways prior to clearing the phlegm from your chest. |
Nebuliser |
|
Hypertonic Saline 7% nebuliser via side stream with a mouthpiece
|
Airway Clearance Techniques: Pari OPEPThe aim of airway clearance is to gather as much phlegm as possible and cough it out in a controlled and energy efficient way. The aim is to clear your chest so you can breathe more freely and still have energy to do the activities you like afterwards.
|
|
Step 1: Start off your airway clearance by doing some long, slow, deep breaths in and out while sat up. Sigh and ‘actively’ let go of the breath – do approx. 5 breaths before moving on to step two.
Then try lying on your side
Step 2; Pari OPEP Try to take a SLOW deep breath in through your nose, filling your lungs as much as possible. Blow out a long, slow breath through your OPEP; try to make the duration of the breath in and out last as long as you can, blow out as far as you can without coughing. Try to keep your cheeks stiff and feel the vibrations deep into your chest. Repeat several of these large breaths to fill your lungs then move on to try some smaller breaths. You can do this by doing a SMALL slow breath in, then blow out through your OPEP device, a low force, long breath out– blow out as far as you can without coughing. Take a small or half sized breath in and continue to blow out as far as you can without coughing. The Pari O-PEP helps to splint open the smaller airways during your breath out, making the diameter of the airway bigger, allowing for more space and stopping the phlegm from getting trapped in the smaller airways. The O-PEP also creates oscillations or vibrations which create turbulence inside the airways, these shearing forces unstick the phlegm and drag it up to the larger airways where it can be coughed up and out of chest.
Step 3: Clearing As you feel the sputum move up try a little huff and a cough. To huff take a breath in and then blow out a forceful, short and fast breath, out through an open mouth. Try a long slow ‘garlic breath’ huff or a short, sharp fast huff.
Postural Drainage; Repeat the cycle above on the opposite side.
Once your breathing has recovered repeat step 2 and 3 until your chest feels clear. Remember- Try to control your cough- control your breath in after your cough so it is not a fast, sharp breath in.
Excessive coughing can lead to increased airway irritability and increase wheeze or chest tightness, if you don’t cough anything up after one or two coughs you should return to more breathing exercises to move the phlegm a little higher before trying to cough again. |
Notes |
|
Repeat your appropriate inhaler, nebulisers and airway clearance twice each day, once in the morning and once in the evening as discussed at your appointment. Remember to wash your OPEP and nebuliser equipment in hot soapy water and leave to air dry.
|
Hypertonic Saline is a drug taken through a nebuliser that you inhale, it has a high salt concentration which acts on the layers of mucus in your airways. It is a mucolytic which means it helps you to clear the phlegm out of your chest, you may have already tried it if you have done a sputum induction procedure with the physiotherapists in clinic. Mucolytics disrupt the structure of the mucus gel, thereby reducing its viscosity and elasticity. The intention of mucolytic therapy is therefore to make the viscoelasticity of the airway secretions better to help their clearance from the airways.
7% Hypertonic Saline Nebusal video: https://youtu.be/wTOpTnhA6no (Other concentrations and brands are available)
The Pari O-PEP device is an Oscillating Positive Expiratory Pressure device which helps with airway clearance, there are several types of adjuncts and breathing techniques which can help you clear your chest. Your physiotherapist will take into account your how much sputum you have, how your airways react to huffing and coughing and your chest xrays and CT reports when deciding which airway clearance technique should work best for you. There are techniques such as the Active Cycle of Breathing Techniques, Autogenic Drainage, Postural Drainage and other devices such as the Aerobika or Acapella Choice.
Aerobika Airway Clearance Adjunct Video: https://youtu.be/iy2oYadhF9Q
Research studies have shown that regular chest clearance treatment assisted with hypertonic saline will make your sputum (phlegm) easier to cough up. This means:
• you may have fewer flare ups of your chest
• you may have fewer admissions to hospital
• your symptoms may improve
• your lungs may stay healthier for longer
• maintain or improve your lung function
Your physiotherapist can help make you a personalised chest maintenance routine to optimise your chest clearance. Do not hesitate to ask the team if you wish to speak with the physiotherapy team at your clinic next appointment.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]

