The Role of Speech & Language Therapy (SALT)
Did you know Speech and language therapists (SLTs) play a crucial role in the management of patients with respiratory conditions?
The Royal College of Speech and Language Therapists (RCSLT) comprehensive factsheet on Upper Airway Disorders (UADs), is an essential guide designed for patients managing chronic respiratory conditions such as CPA, ABPA, COPD, asthma, and bronchiectasis. This resource aims to highlight the often-overlooked possibility of co-existing upper airway disorders, which can significantly complicate the management and treatment outcomes of these chronic respiratory diseases.
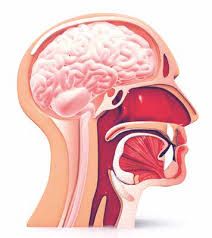
Within these pages, you will find detailed insights into the symptoms, diagnostic challenges, and effective management strategies for UADs. The leaflet emphasises the critical role of Speech and Language Therapists (SLTs) in assessing and treating these disorders. SLTs are key to providing targeted interventions that can alleviate symptoms and improve daily life.
This leaflet also aims to raise awareness amongst clinicians about the importance of considering UADs in the differential diagnosis of respiratory conditions. Enhanced understanding of these disorders can lead to better patient outcomes and improved quality of life.
To access the leaflet, click here.
Understanding How Our Lungs Fight Fungus
Airway epithelial cells (AECs) are a key component of the human respiratory system: The first line of defence against airborne pathogens such as Aspergillus fumigatus (Af), AECs play a crucial role in initiating host defence and controlling immune responses and are important in maintaining respiratory health and preventing infections that can lead to conditions such as aspergillosis. Research by the University of Manchester’s Dr Margherita Bertuzzi and her team sought to understand how AECs combat Af and what leads to vulnerabilities in these defences, particularly in individuals with underlying health conditions.
Previous work by Dr Bertuzzi and her team demonstrated that AECs are effective in stopping the fungus from causing harm when they are functioning well. However, in people who are at higher risk, like those with weakened immune systems or existing lung conditions, if these cells are not working correctly, the fungus can take advantage of this situation.
This new research by Dr Bertuzzi and her team aimed to explore how AECs stop the fungus in healthy people and what goes wrong in people who get sick. The team looked closely at the interaction between the fungus and lung cells from both healthy individuals and those with certain diseases. Using advanced scientific methods, the team was able to observe the interactions between the lung cells and the fungus at a very detailed level.
What They Found
Experiments showed that the stage of fungal growth was important and a surface carbohydrate – mannose (a sugar) also had a role in the process.
Specifically, they discovered that the fungus is more likely to be taken up by lung cells when it has been growing for a few hours compared to when it’s just a fresh spore. Swollen fungal spores that were locked at 3 and 6 hours of germination were 2-fold more readily internalised than those locked at 0 hours. They also identified that a sugar molecule called mannose on the surface of the fungus plays a big role in this process.
Mannose is a type of sugar molecule that can be found on the surface of various cells, including those of pathogens like Aspergillus fumigatus. This sugar plays an important role in the interactions between the fungus and the host’s cells, particularly the AECs lining the lungs. In a healthy immune response, mannose on the surface of pathogens can be recognised by mannose receptors on immune cells, triggering a series of immune responses aimed at eliminating the pathogen. However, Aspergillus fumigatus has evolved to exploit this interaction, allowing it to adhere to and invade lung cells more effectively. The presence of mannose on the fungus’ surface facilitates its binding to mannose-binding lectins (MBLs) (proteins that bind specifically to mannose) on the surface of lung cells. This binding can promote the internalisation of the fungus into the lung cells, where it can reside and potentially cause infection.
The research highlighted the possibility of manipulating this interaction as a means to combat fungal infections. By adding mannose or mannose-binding lectins like Concanavalin A, researchers could significantly reduce the fungus’s ability to invade lung cells. This reduction was accomplished by essentially “competing” with the fungus for the binding sites on the lung cells or by directly blocking the fungal mannose, thereby inhibiting the interaction that facilitates fungal infection.
Why does it matter?
Understanding these interactions gives us important insights into how our lungs protect us from fungal infections and what goes wrong in people who are vulnerable to such infections. This knowledge could help in creating new treatments against pathogens like Aspergillus fumigatus.
You can read the full abstract here.
Celebrating British Science Week: The Vital Role of the Mycology Reference Centre Manchester
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.24.2" _module_preset="default"][et_pb_row _builder_version="4.24.2" _module_preset="default" theme_builder_area="post_content"][et_pb_column _builder_version="4.24.2" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.24.2" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0"]
British Science Week presents the ideal opportunity to highlight the exceptional work of our colleagues at the Mycology Reference Centre Manchester (MRCM). Renowned for its expertise in diagnosing, treating, and researching fungal infections, the MRCM has made vital contributions to fungal diagnostics and patient care. In 2017 the centre was designated a European Confederation of Medical Mycology (ECMM) Centre of Excellence in Clinical and Laboratory Mycology and Clinical Studies. This designation was further extended in 2021, highlighting the MRCM's dedication to advancing research capabilities, enhancing resources, and fostering international collaboration. Such efforts contribute to the development of services and ensure that the MRCM remains at the forefront of medical mycology, setting standards for diagnostic excellence and patient care.
Located at Wythenshawe Hospital and operating under the Manchester University NHS Foundation Trust (MFT), the Mycology Reference Centre Manchester (MRCM) provides specialist mycology diagnostic services within Greater Manchester and throughout the UK. The centre offers an extensive range of services, including antifungal management and mycological guidance on diagnosing diseases and clinical management and care of patients. Their expertise covers a broad spectrum of conditions, including Candida infections and chronic and invasive Aspergillus infections, in addition to addressing issues related to moulds in homes and their impact on human health.
The importance of the MRCM's work extends beyond diagnosis. Fungal infections, with their ambiguous symptoms, require a combination of clinical observation and laboratory investigation for accurate identification and treatment. The MRCM's accredited diagnostic work provides clarity and direction for effective patient management.
Moreover, the MRCM, in collaboration with the National Aspergillosis Centre, contributes significantly to the academic sphere. Both centres work with the University of Manchester Fungal Infection Group (MFIG) and play a vital role in the education and training of future medical professionals through undergraduate and post-graduate programmes in Medical Mycology and Infectious Diseases. This educational role ensures high-quality training for professionals entering the field, further strengthening the UK's capacity to combat the growing problem of fungal diseases and antimicrobial resistance.
The Mycology Reference Centre Manchester is a cornerstone for fungal diagnostics, a hub for international training and research, and a critical partner in the global fight against fungal infections. As we celebrate British Science Week, we would like to take the opportunity to acknowledge and commend the work of our colleagues at the MRCM and their invaluable contributions to science, medicine, and patient care both nationally and internationally.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Harnessing the Power of a Symptom Diary: A Guide to Better Health Management.
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.24.2" _module_preset="default"][et_pb_row _builder_version="4.24.2" _module_preset="default" theme_builder_area="post_content"][et_pb_column _builder_version="4.24.2" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.24.2" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0"]
Managing a chronic condition can be a challenging journey filled with uncertainties. However, there is a tool that can help patients take control of their condition and help them understand potential triggers and how lifestyle factors may impact their condition. This tool comes in the form of a symptom diary, a personal record that tracks information relevant to the patient, such as symptoms, ad hoc medication usage, exacerbations, food intake and activities.
Key benefits are:
- Empowerment and control are at the core of why keeping a symptom diary is beneficial. It offers individuals a sense of ownership over their health, allowing them to monitor and manage their condition, rather than feeling overwhelmed by it. This proactive approach is not only beneficial for the patient's sense of well-being but also contributes to research and future planning. Documenting symptoms can help better understand the condition, aiding not just the individual but also the broader community by contributing valuable insights into chronic illness management.
- Another benefit of maintaining a symptom diary is its ability to foster improved communication between patients and their medical teams. By providing a detailed account of symptoms and their impacts, a diary ensures that important information is communicated effectively, allowing for a focused discussion during appointments. This enhanced communication can lead to more informed and focused care, concentrating on what truly matters to the patient's health and well-being.
- Beyond facilitating better dialogue, a symptom diary promotes self-awareness through monitoring and reflection, patients may notice patterns in their symptoms, identifying what exacerbates or alleviates their condition. This awareness is crucial in managing chronic illnesses like aspergillosis, as it empowers patients to make informed decisions about their health.
- A symptom diary can also play a role in developing personalised treatment plans. Each entry can help the clinical team better understand the patient's condition, enabling in some circumstances the creation of a treatment strategy that is as unique as the individual. This tailored approach can improve health outcomes, making a difference in the patient's quality of life.
Starting a symptom diary involves a few key practices: maintaining consistency in entries, attention to detail, and regularly reviewing the diary to identify trends or changes. What to record in a diary includes the date and time of each entry, detailed symptoms, ad hoc medication usage, environmental exposures, dietary intake, physical activity, mental health, and sleep quality.
In conclusion, a symptom diary is a powerful tool in managing chronic conditions, offering benefits such as improved communication with healthcare providers, increased self-awareness, empowerment, and the facilitation of personalised treatment plans. By taking control of their health information, individuals can navigate their journey with confidence and clarity, paving the way for a better quality of life.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Patient Reflection on Research: The Bronchiectasis Exacerbation Diary
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.24.2" _module_preset="default"][et_pb_row _builder_version="4.24.2" _module_preset="default" theme_builder_area="post_content"][et_pb_column _builder_version="4.24.2" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.24.2" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0"]
Navigating the rollercoaster of chronic illness is a unique and often isolating experience. It is a journey that can be filled with uncertainties, regular hospital appointments, and a never-ending quest for a return to normal. This is so often the reality for individuals with chronic respiratory diseases, such as aspergillosis.
In this post, Evelyn embarks on a reflective journey, chronicling the evolution of her illness from childhood diagnosis to the present day, a timeline characterised by bilateral severe cystic bronchiectasis complicated by the colonisation of aspergillus and the less common scedosporium. For Evelyn, keeping a diary, noting symptoms, infections, and treatment strategies has been a way to make sense of the unpredictability of her health. This habit, instilled years ago by a forward-thinking consultant, transcends its practical utility, evolving into a critical tool for patient empowerment and self-advocacy.
When searching the web for help refining her symptom diary, Evelyn came across a paper titled: The Bronchiectasis Exacerbation Diary. This paper was a revelation of sorts. It cast light on often-overlooked aspects of the patient-experience and validated the often inexplicable symptoms that Evelyn experiences. It is evidence as to the power of patient-centered research and the impact of seeing lived experience acknowledged in scientific literature.
Evelyn's below reflection is a reminder of the broader implications of chronic illness on daily life and the need to adapt to navigate daily life.
As a result of a conversation with Lauren recently concerning the use of a symptom diary/journal, I came across a paper published on the internet, ‘The Bronchiectasis Exacerbation Diary’. Diagnosed in childhood with a chronic respiratory disease which has progressed throughout my life, I have bilateral severe cystic bronchiectasis with colonisation of aspergillus and the rarer fungi, scedosporium.
I have long been accustomed to keeping notes of symptoms/infections/treatment, having been encouraged to do so, many years ago, by a consultant for ease of reference at appointments. He emphasised treating infections should be dependent on the result of a sputum culture and sensitivity and not on a “Russian roulette” approach, as he called broad spectrum antibiotics; without knowing what type of infection was involved. Thankfully, my GP was co-operative, as at that time cultures were not routine. (I had dreaded acquiring a reputation as a bolshie patient!)
Reading the above mentioned paper was a revelation. It brought together the range of symptoms I experience daily, even some symptoms I felt were not appropriate to mention at clinic consultations. Moreover, I felt validated.
There have been occasions, albeit rarely, when I have doubted myself, none more so than when one clinician inferred I was psychosomatic. This was my lowest point. Thankfully, following this I was referred to a respiratory physician at Wythenshawe Hospital who, when a culture showed aspergillus, transferred me to Professor Denning’s care; as they say “every cloud has a silver lining”. Aspergillus had previously been found in a culture at another hospital in 1995/6, but not treated in the way it was at Wythenshawe.
Not only everyday symptoms were considered in the article, but also the immediate impact patients’ experience with daily living. Also, in a wider sense, the general impacts on our lives and the adjustments we all face in coping – all of which I can so easily identify with in my own life.
I felt so encouraged reading the paper as despite all of the various types of patient information leaflets I have read through the years, none were so comprehensive.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Empowering Patients through Understanding Professional Medical Guidelines
[et_pb_section fb_built="1" _builder_version="4.24.0" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_row _builder_version="4.24.0" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.24.0" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_text _builder_version="4.24.0" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"]
Navigating the healthcare landscape can be daunting for patients and their families, especially when dealing with complex lung conditions like aspergillosis. Understanding medical jargon and diagnostic and treatment paths is often overwhelming. This is where the European Lung Foundation (ELF) can help with its initiative to demystify professional medical guidelines.
The Importance of Lay Versions of Guidelines
The ERS provides detailed clinical guidelines for healthcare professionals, outlining the best practices in the diagnosis, management, and treatment of various lung conditions. However, these documents are often technical and challenging for non-clinical people to understand. Recognising this gap, the ELF has produced lay versions of these guidelines. These simplified versions can help support patient education and empower individuals to understand their health conditions better.
Why Patients Should Utilise These Guidelines:
- Enhanced Patient Engagement: Understanding these guidelines enables patients to actively participate in their healthcare decisions.
- Improved Communication with Clinicians: Patients who understand the guidelines can communicate more effectively with their doctors, leading to better healthcare outcomes.
- Empowerment in Managing Health: Knowledge of treatment standards and protocols allows patients to advocate for their health and ensures they receive the best possible care.
The Role of Guidelines in Healthcare
Clinical guidelines are vital in ensuring consistency and quality in healthcare. They provide a framework for healthcare professionals to deliver the most effective treatments based on the latest research and best practices.
The ELF's effort in translating professional guidelines into layman's terms is a commendable step towards patient empowerment. By understanding these guidelines, patients and their caregivers can navigate the healthcare system more effectively, ensuring they receive the best possible care for their lung conditions.
We encourage patients, their carers and families to explore these resources provided by the European Lung Foundation to better understand their health conditions and treatment options.
You can access the guidelines by visiting here.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Thoughts on the Aspergillosis Journey Five Years On - November 2023
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.23.1" _module_preset="default"][et_pb_row _builder_version="4.23.1" _module_preset="default" theme_builder_area="post_content" custom_margin="50px|auto|50px|61px|true|false" custom_padding="0px|1px|0px|0px|false|false" width="90.7%"][et_pb_column _builder_version="4.23.1" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.23.1" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0" width="99.9%"]
Alison Heckler ABPA
I have written about the initial journey and diagnosis before, but the ongoing Journey occupies my thoughts these days. From a Lung/Aspergillosis/ Breathing perspective, now that we are coming into summer in New Zealand, I feel I’m doing ok, looking and feeling well.
Some of my current Medical Background:-
I started the biologic, mepolizumab (Nucala), in September 2022 after a really difficult 12 months (another story). By Christmas, I was much improved and, from a breathing and energy perspective, had a good summer; although the weather was so bad, it was hardly a summer.
I got complacent about precautions, and in early February, a grandson visited with what turned out to be a nasty flu that I then went down with. 6 weeks later, a follow-up X-ray on the lungs showed a heart issue that needed a cardiologist to check “well the aortic stenosis isn’t a big worry but the aortic duct never healed over as a child. We could repair but …..” the answer to that was “I’m over 70, had four pregnancies, I’m still here & the risk factors with all my other issues ….. not going to happen”
Once finally over those two hiccups, my 81-year-old sister was admitted to the hospital, and I was trying to advocate for her. She got Covid, which I subsequently got from her. (I had done well to stay Covid Free for 2.5 years). But yet again, any infection I get these days takes much longer to recover from; I still had it at four weeks, and at 6-8 weeks, my GP was concerned that I might have developed Long Covid as my BP and heart rate were still a bit on the high side! My sister was diagnosed with Myeloma and died within six weeks of diagnosis.
Since starting the Mepolizumab, I had noticed increasing problems with incontinence, and this developed in a full-blown Pyelonephritis (eColi Kidney Infection). As I only have one kidney, the anxiety level over this was a bit high as the symptoms were/are all very similar to when my other kidney was eventually removed. (No plan B here). Toss-up: able to breathe versus learning to deal with some incontinence?
I overlay all of 2023 with ongoing Mental Health issues with my 13-14-year-old granddaughter, so my daughter and her husband, on whose property I live, were totally preoccupied with trying to keep her safe and all the care that she requires. We are all grieving the loss of this child who is now in care.
Pain levels are high, and energy levels are very low. Prednisone has essentially killed my cortisol production, so I have Secondary Adrenal Insufficiency and Osteoporosis.
But I am Thankful
I am so grateful that I am blessed to live in a country that has a Public Health System (be it a similarly crumbling one as NHS). I was able to move to an area that has a good teaching hospital and be close to my daughter (Palliative Care physician) & her husband (Anaesthetist), I have access to free public health medications and an excellent GP who listens, looks at the whole picture and does her best to get all the Specialist to review the situation. Recent x-rays and Dexta Scan revealed the extent of the damage and deterioration of the spin: Info I need to bring to the attention of the Physio who is trying to help with my motivation/activation of strengthening exercises. Endocrinology suggested a 5mg increase in my hydrocortisone and a pushing out of the dose timing, and that has made a HUGE difference in how I cope with dealing with all that is going on and the pain. Urology has finally accepted a referral to review my kidney situation, although it still might be a few months before they see me. A recent checkup with the Physio found that the exercises had made a difference, and I was considerably stronger in my legs. I still struggle to do these, but this information informs me that I need to persist.
The Biggest Battle is Mental Attitude
Each of our stories will be unique, and for each of us, the battle is real. (When I write mine all down, it does sound a bit overwhelming, but generally, I don’t think of it in that way. I have shared my story only as an example of the complexity of the journey.)
How do we cope with all of the changes that come upon us? I knew that my health would change as I got older, but I feel like it has come upon me so rapidly. I didn’t think of myself as old, but my body is most definitely thinking and behaving that way!
Learning to:
Accept the things I cannot change,
to Work on the things I can change,
And the wisdom to know the difference
This process of letting go of dreams and hopes and setting new, more modest goals has been important. I have learned that after a more strenuous activity (by my current abilities), I have to sit down and rest or do something that allows me to rest and be productive. I have previously been somewhat of a ‘workaholic’ and not much of a planner, so this transition has not been easy. All of these changes are a Grieving Process, and like any grief, we heal better if we acknowledge it for what it is, then we can learn to live with our grief. We can move forward into all the ‘new normals’. I now have a planning diary with notes on what I want/need to do, but it is not planned out in detail as I have to “go with the flow” as it were on how much energy I have available to get things done. The reward is that I will eventually get things ticked off. If it’s only 1 or 2 daily tasks, that’s ok.
When I finally got a diagnosis in 2019, I was told that “it was not lung cancer; it was ABPA, which is chronic and incurable but could be managed”. What ‘be managed’ entailed, I most definitely did not take in at the time. Every medication that we take is going to have a side effect; antifungals and prednisone are way up there in that respect, and it is sometimes the side issues that are more difficult to cope with. Mentally, I have to remind myself that I can breathe and haven’t died of secondary pneumonia because of the meds that keep the aspergillosis under control. I am alive because I manage my intake of Hydrocortisone every day.
Weighing up the benefits versus the side effects. There are some medications that once I studied the side effects and contraindications and weighed that info against the benefits for relieving Peripheral Neuropathy, I consulted with a Dr, and we dropped it. Other medications do have to stay, and you learn to live with the irritations (rashes, dry skin, extra back pain, etc.). Again, we are each unique in what we can manage, and sometimes, it is the attitude (stubbornness) with which we approach the situation that will determine our direction.
A note on stubborn…. Last year, I set myself the goal of getting my daily average walking distance back up to 3k per day. It was a bit of a mission when some days I wasn’t reaching 1.5K. Today, I managed a 4.5 flat walk on the beach and, more importantly, saw the daily average over the past 12 months get to 3k per day. So, I celebrate a win for as long as it lasts. I make clip-on pouches for my iPhone so that I always carry it to record my steps, and I recently purchased a Smart Watch that includes recording all my health data statistics. It is a new normal to track this stuff, and the NAC research Team is wondering if such data could help us predict ABPA flares etc.
For me, my faith in the sovereignty of God is paramount in keeping me focused and moving forward.
“He knit me together in my mother's womb. My days are ordered by his hand.” Psalm 139.
I have been saved by Grace, by Christ alone.
Yes, a number of my medical conditions could/will contribute to my death; we all die at some point, but I can live the best life I can now, knowing that God still has work for me to do.
“This world is not my home. I’m just a passing through.”
Talking with others on Teams Video and reading posts or stories on Facebook Support or the website all add to helping me keep positive. (At least most of the time) Hearing other people's stories helps to put my own back into perspective … I could be worse. So, as best I can, with the Lord’s help, I hope to encourage others to keep walking on the difficult road you sometimes find yourself on. Yes, it can be very difficult at times, but look at it as a new challenge. We are not promised an easy life.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Do you have asthma and Allergic Bronchopulmonary Aspergillosis?
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.23" _module_preset="default"][et_pb_row _builder_version="4.23" _module_preset="default" theme_builder_area="post_content" width="91.8%"][et_pb_column _builder_version="4.23" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.23" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0"]
We're excited to share that there's a new clinical study that's looking into an innovative treatment specifically for individuals dealing with both asthma and ABPA. This treatment comes in the form of an inhaler called PUR1900.
What is PUR1900?
PUR1900 is an inhaled medication that's being tested for its effectiveness against the symptoms of ABPA in asthma patients. It’s designed to deliver an antifungal medication directly to the lungs, where it can work right at the source of the problem.
The Study at a Glance
The study spans several months and is divided into three key phases:
- Screening Period (28 days): Researchers will do some tests to make sure this study is the right fit for you.
- Treatment Period (112 days): If you're eligible, you'll use the inhaler for about 16 weeks. You could receive either a higher dose, a lower dose of PUR1900, or a placebo (which doesn't contain the actual medication).
- Observation Period (56 days): After the treatment, researchers will keep an eye on your health for another 8 weeks.
What Will Participants Do?
- Daily Routines: You'll use the inhaler daily as directed and keep track of your experience in an electronic diary (eDiary).
- At-Home Checks: You'll measure your breathing strength daily using a simple device.
- Clinic Visits: Approximately once a month, you'll visit the clinic for check-ups and tests.
Why Participate?
By joining this study, you're not only potentially finding a new way to manage your asthma and ABPA, but you're also contributing to medical research that could help countless others in the future.
Safety and Benefits
Your safety is the top priority. You'll be closely monitored throughout the study, and all treatments will be provided at no cost to you. Plus, if you successfully complete the study, there may be an opportunity to continue receiving PUR1900 in a follow-up study.
Taking the Next Step
Researchers are looking for adults with asthma and ABPA who are interested in exploring this new treatment option. If you're ready to take the next step, eligibility and contact details on how you can participate in this groundbreaking study can be found by clicking here.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
The Marathon of Management: Steady Pacing Through Chronic Condition Flares
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.23" _module_preset="default"][et_pb_row _builder_version="4.23" _module_preset="default" theme_builder_area="post_content" width="93.3%"][et_pb_column _builder_version="4.23" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.23" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0"]
Living with a chronic condition is like navigating a course with varied terrain. It's not a journey that will end in recovery in the conventional sense, as the condition itself persists. Instead, it is about managing the fluctuations—periods of stability interspersed with challenging exacerbations or complications like infections or additional illnesses.
In the world of distance running, there's a strategy known as "go slow to go fast." It's a principle that initially seems counterintuitive; to achieve speed and efficiency in a race, a runner must first invest time in slow, steady-paced training. But, in running, this approach builds a robust foundation of aerobic fitness, reducing injury risk and preparing the body for the demands of faster running in the future. In essence, "go slow to go fast" is not just about running—it's a metaphor for any process that requires building strength and resilience, one step at a time, and for individuals navigating the complexities of chronic conditions, adopting this philosophy could help manage their health over time by learning to listen to their body and respecting its need for gradual progression. Just as runners build their pace over time to avoid burnout, patients could benefit from looking at their journey with patience and persistence—understanding that managing a chronic condition often requires a slow and steady approach to maintain health and prevent exacerbations.
Setting Achievable Goals
After a flare-up, complications or other illnesses, it's important to reassess and set realistic goals tailored to current capabilities. Like a runner adjusting their training post-injury, patients must recalibrate their expectations and focus on attainable health milestones - no matter how small. Adapting goals accordingly can help to maintain progress without overstepping physical limits.
Crafting a Personalised Management Plan
Chronic conditions require a personalised management plan, one that considers the unpredictability and variability of symptoms. Drawing on a parallel with a runner's individualised training regime, patients can benefit from a bespoke plan that accommodates their fluctuating health, devised with input from healthcare professionals.
Embracing Consistency and Patience
Consistent management and the patience to accept slower progress at times are essential when living with a chronic condition, and symptoms will often present challenging days; finding strength in routine and maintaining a slow and steady approach on these days is important.
Recognising and Celebrating Progress
In the marathon that is chronic condition management, small victories can be profound. Celebrating the days when symptoms are managed effectively or when you can do that little bit more will bolster spirits and encourage continued effort.
Adjusting to Health Fluctuations
Just as a runner must listen to their body and adjust their training accordingly, patients with chronic conditions must remain flexible, adapting their management strategies in response to changes in their health - even if this means scaling back activities on a bad day.
Leaning on Your Support Team
The role of a support system is indispensable when living with a chronic illness. The encouragement from healthcare providers, family, and support groups can provide immense comfort and practical help during more challenging times.
Envisioning Your 'Finish Line'
While there may not be a traditional 'finish line' in chronic condition management, defining personal milestones and envisioning moments of reprieve can be incredibly motivating. Each phase of improved health or successful adaptation to a health challenge can be seen as its finish line, a testament to the patient's resilience.
The metaphor "go slow to go fast" transcends the realm of running. It can offer a powerful perspective for those managing chronic conditions like aspergillosis. It's a reminder that resilience often requires a measured approach, where understanding limits and gradually extending them is key to sustainable health management. This journey, punctuated by careful pacing and an awareness of our bodies, allows for periods of rest and recovery, which are just as important as the times of activity and progress. By embracing this principle, individuals can navigate their health challenges and build towards better days with confidence. While the finish line may differ in this marathon of management, each step taken at the right pace is a stride towards living a fuller life, regardless of the terrain ahead.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Expanded NHS support available for patients in GP practices across the country
[et_pb_section fb_built="1" _builder_version="4.23" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_row _builder_version="4.23" _module_preset="default" width="93.9%" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.23" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_text _builder_version="4.23" _module_preset="default" width="100%" hover_enabled="0" global_colors_info="{}" theme_builder_area="post_content" sticky_enabled="0"]
Did you know that a visit to your local GP practice now comes with an added layer of healthcare support? Under the newly rolled out GP Access Recovery Plan by the NHS, your local GP practice has additional healthcare staff and services designed to provide comprehensive care right in your community.
Here’s a breakdown of the new additions:
More Hands on Deck:
Since 2019, over 31,000 extra healthcare staff have joined general practices across the nation. This means besides your GP or practice nurse, there's now a diverse team of healthcare professionals, including pharmacists, mental health practitioners, paramedics, and physiotherapists, available to cater to your health needs.
Direct Access to Specialised Care:
When you contact your practice with a health issue, there’s a trained team ready to assess your needs and direct you to the right professional. For instance, if you have muscular pain, you’ll be booked to see a physiotherapist straight away.
No GP Referral? No Problem:
You don't always need a GP referral to see certain healthcare specialists. Now, you can get specialist support from mental health professionals, physios, and pharmacists without having to see a GP first. This is all about getting you the right care, faster.
Digital Doorway to Your GP:
32 million people use the NHS app to book appointments or check test results. This digital tool simplifies how you reach out to your GP, making healthcare access easier.
Social Prescribing for Holistic Care:
Social prescribing link workers can help with non-medical issues, like loneliness or financial advice. They even run community-based courses to impart new skills. For instance, in Nottingham, patients were able to learn cooking skills, opening doors to new opportunities.
Knowledge is Power:
A recent survey revealed that one in three people in England are still unaware of these upgraded services at their GP practice. Spreading the word ensures that more individuals can benefit from the expanded support available.
The enhanced support at GP practices is a significant stride towards creating a robust, community-centred healthcare system. It’s all about ensuring that you receive the right care, from the right professional, at the right time.
If you want to know more, visit nhs.uk/GPservices to explore the expanded services available at your GP practice.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
