A Breath of Fresh Air: Repairing COPD Damage with Patients' Own Lung Cells
[et_pb_section fb_built="1" _builder_version="4.23" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_row _builder_version="4.23" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.23" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_text _builder_version="4.23.1" _module_preset="default" hover_enabled="0" global_colors_info="{}" theme_builder_area="post_content" sticky_enabled="0"]
In a remarkable advancement towards treating Chronic Obstructive Pulmonary Disease (COPD), scientists have, for the first time, demonstrated the potential of repairing damaged lung tissue using patients' own lung cells. The breakthrough was unveiled at this year's European Respiratory Society International Congress in Milan, Italy, where results from a pioneering phase I clinical trial were shared.
COPD, which is common in those with chronic pulmonary aspergillosis (CPA), causes progressive damage to lung tissue, significantly impacting the quality of life for patients through the obstruction of airflow out of the lungs. The disease, claiming the lives of roughly 30,000 people in the UK each year, has been historically challenging to treat. Current treatments mainly focus on alleviating symptoms through bronchodilators such as salbutamol, which widen the airways to enhance airflow but do not repair the damaged tissue.
The search for a more definitive treatment led researchers to explore the realms of stem cell and progenitor cell-based regenerative medicine. Stem cells are known for their ability to morph into any cell type. Unlike stem cells, progenitor cells can only turn into certain types of cells related to a specific area or tissue. For example, a progenitor cell in the lung can turn into different types of lung cells but not into heart cells or liver cells. Among the researchers is Professor Wei Zuo from Tongji University, Shanghai and chief scientist at Regend Therapeutics. Professor Zuo and his team at Regend have been investigating a specific type of progenitor cell known as P63+ lung progenitor cells.
20 COPD patients were enrolled in the trial, 17 of whom received the cell treatment, while three served as the control group. The results were encouraging; the treatment was well tolerated, and patients exhibited improved lung function, could walk further, and reported a better quality of life following the treatment.
After 12 weeks of this new treatment, patients experienced a significant improvement in their lung function. Specifically, the lungs' ability to transfer oxygen and carbon dioxide to and from the bloodstream became more efficient. Additionally, patients could walk further during a standard six-minute walking test. The median (the middle number when all numbers are arranged from smallest to largest) distance increased from 410 meters to 447 meters - a good sign of improved aerobic capacity and endurance. Moreover, there was a notable decrease in the scores from the St George’s Respiratory Questionnaire (SGRQ), a tool used to measure the impact of respiratory diseases on overall quality of life. A lower score indicates that patients felt their quality of life had improved, with fewer symptoms and better daily functioning. Overall, this suggests that the treatment improved lung function and positively impacted patients' day-to-day lives.
The groundbreaking results also highlighted the potential of this treatment in repairing lung damage in patients with mild emphysema (a type of lung damage that occurs in COPD), a condition generally considered irreversible and progressive. Two patients enrolled on the trial with the condition showed resolution of the lesions at 24 weeks by CT imaging.
Endorsed by China's National Medical Products Administration (NMPA), which is the equivalent of the UK Medicines and Healthcare products Regulatory Agency (MHRA), a phase II clinical trial is in the pipeline to test further the use of P63+ progenitor cell transplantation in a larger group of COPD patients.
This innovation could significantly alter the course of treatment in COPD. Professor Omar Usmani of Imperial College London and Head of the European Respiratory Society group on airway disease, asthma, COPD and chronic cough provided his thoughts on the trial's significance, underscoring the urgent need for more effective treatments for COPD. He noted that if these results are confirmed in subsequent trials, it would be a major breakthrough in COPD treatment.
The road ahead appears promising, with the potential to not only alleviate the debilitating symptoms of COPD but to repair the damage it inflicts on the lungs, offering hope to millions suffering from this chronic respiratory disease.
You can read in more detail about the trial here: https://www.ersnet.org/news-and-features/news/transplanting-patients-own-lung-cells-offers-hope-of-cure-for-copd/
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Empowering Yourself: Recognising Heart Attack Symptoms Could Be A Lifesaver
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.22.2" _module_preset="default"][et_pb_row _builder_version="4.22.2" _module_preset="default" theme_builder_area="post_content" custom_margin="50px|30px|50px|45px|true|false"][et_pb_column _builder_version="4.22.2" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.22.2" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0" custom_margin="|-141px||||"]
In the hustle and bustle of our daily lives, we often overlook the subtle signs of illness that our bodies tell us, dismissing minor aches and discomforts. This tendency, however, can prove dangerous, especially when it comes to recognising the symptoms of a heart attack.
A recent survey by NHS England unveils a concerning reality - many individuals are not confident in identifying the signs of a heart attack, with the figures being notably higher among those over 55. This lack of awareness could be a matter of life and death, particularly for individuals with chronic conditions who might misattribute heart attack symptoms to their existing ailments.
The NHS England's 'Help Us, Help You' campaign calls for everyone to equip themselves with the knowledge of heart attack symptoms and act promptly by calling 999 if they suspect they or someone around them is having a heart attack.
Heart attack symptoms can be elusive and may vary from person to person. The most common symptom is chest pain, often described as a feeling of pressure, heaviness, tightness, or squeezing across the chest. However, symptoms can also manifest in other forms, such as pain in the arms, jaw, neck, back, and tummy, lightheadedness, sweating, shortness of breath, nausea, vomiting, an overwhelming feeling of anxiety, coughing or wheezing.
The narratives of heart attack survivors Asif and Gemma underscore the importance of heeding these signs. Gemma initially dismissed her symptoms as exercise-induced discomfort, while Asif mistook his for food poisoning. Their stories are a stark reminder that a delay in seeking help can result in severe heart muscle damage, impacting the quality of life post-recovery.
For individuals managing chronic conditions, it's easy to fall into a routine of attributing all discomfort to the existing ailment. This mindset, however, can obscure the onset of other serious conditions like a heart attack. Listening to your body, understanding its signals, and seeking medical attention when something feels amiss is imperative.
The campaign by NHS England also sheds light on the common confusion between heart attacks and cardiac arrests. While a heart attack is a circulation problem caused by a blockage that inhibits blood flow to the heart, a cardiac arrest is an electrical issue where the heart suddenly stops beating. Understanding this distinction is crucial as the immediate response required for each differs significantly.
The 'Help Us, Help You' campaign is more than just a slogan; it's a plea for public vigilance and a step towards fostering a culture of proactive healthcare. By educating ourselves and acting promptly, we safeguard our health and contribute to a community where timely intervention becomes a norm rather than an exception.
With over 84,000 hospital heart attack admissions in England during 2021/22, the urgency of this message cannot be overstated. Visit nhs.uk/heartattack for further information. Your prompt action could be a beacon of hope for yourself and others, ensuring that heartbeats continue to echo with vitality.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Understanding the UK Government's New Guidance on Damp and Mould: What It Means for Tenants and Landlords
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.22.2" _module_preset="default"][et_pb_row _builder_version="4.22.2" _module_preset="default" theme_builder_area="post_content"][et_pb_column _builder_version="4.22.2" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.22.2" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0" custom_margin="-75px|-90px||-80px||" custom_padding="0px|||||"]
Understanding the UK Government's New Guidance on Damp and Mould: What It Means for Tenants and Landlords
Introduction
The UK Government has recently published a comprehensive guidance document aimed at addressing the health risks associated with damp and mould in rented homes. This guidance comes as a direct response to the tragic death of 2-year-old Awaab Ishak in 2020, who lost his life due to mould exposure in his family home. The document is a crucial step in ensuring that landlords understand their responsibilities and that tenants are protected from the health risks associated with damp and mould.
The Tragic Catalyst: Awaab Ishak
The guidance was formulated in the wake of the tragic death of Awaab Ishak, a 2-year-old who died due to mould exposure in his family home. The Coroner’s report highlighted a series of failures by the housing provider, leading to this avoidable tragedy. The guidance aims to prevent such incidents from happening again by educating landlords about their legal responsibilities and the serious health risks that damp and mould pose.
Key Messages from the Guidance
Health Risks
The guidance emphasises that damp and mould primarily affect the respiratory system but can also have detrimental effects on mental health. Vulnerable groups, such as children, older adults, and people with pre-existing health conditions, are at greater risk.
Landlord Responsibilities
Landlords are urged to respond sensitively and urgently to reports of damp and mould. They are required to tackle the underlying issues promptly without waiting for medical evidence. The guidance also stresses that tenants should not be blamed for the conditions leading to damp and mould.
Proactive Approach
The guidance encourages landlords to adopt a proactive approach to identifying and tackling damp and mould. This includes having clear processes in place, understanding the condition of their homes, and building relationships with health and social care professionals.
Legal Changes and Future Plans
The government plans to introduce several legislative changes to improve housing standards:
- 'Awaab’s Law': New requirements for landlords to address hazards like damp and mould.
- New powers for the Housing Ombudsman.
- Review of the Decent Homes Standard.
- Introduction of new professionalisation standards for housing staff.
The Significance of the Guidance
For Landlords
The guidance serves as a comprehensive manual for landlords, outlining their legal responsibilities and offering best practices. Failure to adhere to these guidelines could result in legal repercussions.
For Tenants
A Commitment to Health and Well-Being
One of the most significant aspects of the new government guidance is the assurance it provides to tenants. For many renters, particularly those in social housing or in older properties, damp and mould can be persistent issues that are often ignored or inadequately addressed by landlords. The guidance makes it clear that such negligence is not only unacceptable but also illegal. By outlining the health risks associated with damp and mould, from respiratory issues to mental health impacts, the guidance underscores the government's commitment to the health and well-being of tenants.
Empowering Tenants
The guidance serves as an empowering tool for tenants. It provides them with the information they need to understand what constitutes a safe and habitable living environment. This knowledge is crucial when it comes to holding landlords accountable for the conditions of the property. Tenants can now point to a government document that clearly outlines the responsibilities of landlords, thereby strengthening their position in any disputes over property conditions.
A Resource for Legal Recourse
The guidance is not just a set of recommendations; it is tied to legal standards and forthcoming legislation. This means that tenants have a stronger legal footing if they need to take action against a landlord who is failing to maintain a property to the required standard. For example, the introduction of 'Awaab’s Law' will set out new requirements for landlords to address hazards like damp and mould, providing tenants with a specific legal framework to refer to in case of disputes.
Encouraging Proactive Reporting
The guidance also encourages tenants to report issues of damp and mould without fear of blame or repercussions. It explicitly states that damp and mould are not the result of 'lifestyle choices' and that landlords are responsible for identifying and addressing the underlying causes. This is particularly important for tenants who may have been hesitant to report issues in the past due to fear of eviction or other forms of retaliation.
Mental Health Benefits
By addressing the issue of damp and mould, the guidance also indirectly contributes to the mental well-being of tenants. Living in a damp or mouldy home can be a significant source of stress, exacerbating existing mental health issues or contributing to new ones. Knowing that there are guidelines in place to ensure that landlords take these issues seriously can provide tenants with peace of mind.
For Healthcare Providers
Healthcare providers can also benefit from this guidance as it provides valuable information on the health risks associated with damp and mould, aiding in diagnosis and treatment.
Potential Impacts
- Improved Housing Standards: The guidance is expected to raise the bar for housing standards across the UK.
- Better Tenant-Landlord Relations: The clarity provided by the guidance could lead to improved relationships between tenants and landlords.
- Legal Accountability: Landlords are now more accountable, legally, for providing safe and habitable living conditions.
- Public Awareness: The guidance could lead to increased public awareness about the health risks associated with damp and mould.
The UK Government's new guidance on damp and mould is a significant step forward in ensuring safer and healthier living conditions in rented homes. It serves as a vital resource for landlords, tenants, and healthcare providers alike. While it is too early to measure the full impact of this guidance, it holds the promise of instigating positive changes in the UK's housing sector.
You can access a full copy of the guidance via the link below:
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Understanding Sepsis: A Patient's Guide
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.22.2" _module_preset="default" hover_enabled="0" sticky_enabled="0"][et_pb_row _builder_version="4.22.2" _module_preset="default" theme_builder_area="post_content"][et_pb_column _builder_version="4.22.2" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.22.2" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0" custom_margin="0px|-91px||-69px||"]
World Sepsis Day, observed on the 13th of September, united individuals and healthcare professionals worldwide in the fight against Sepsis, which accounts for at least 11 million deaths globally every year. Various healthcare institutions, including the NHS and organisations like the Sepsis Trust, actively participated in spreading awareness about Sepsis, its early signs, and the importance of timely medical intervention.
Facts about Sepsis from the World Sepsis Day Website
CASES & DEATHS
- 47 to 50 million sepsis cases per year
- At least 11 million deaths per year
- 1 in 5 deaths worldwide is associated with Sepsis
- 40% of cases are children under 5
SEPSIS IS THE NUMBER ONE…
- …cause of death in hospitals
- …of hospital readmissions
- …healthcare cost
SOURCES OF SEPSIS
- Sepsis is always caused by an infection – like pneumonia or diarrheal illness
- 80% of sepsis cases occur outside of a hospital
- Up to 50% of sepsis survivors suffer from long-term physical and/or psychological effects
Understanding Sepsis
Sepsis occurs when the body's response to an infection results in damage to its own organs. If left untreated, Sepsis can lead to septic shock, a critical and often fatal condition.
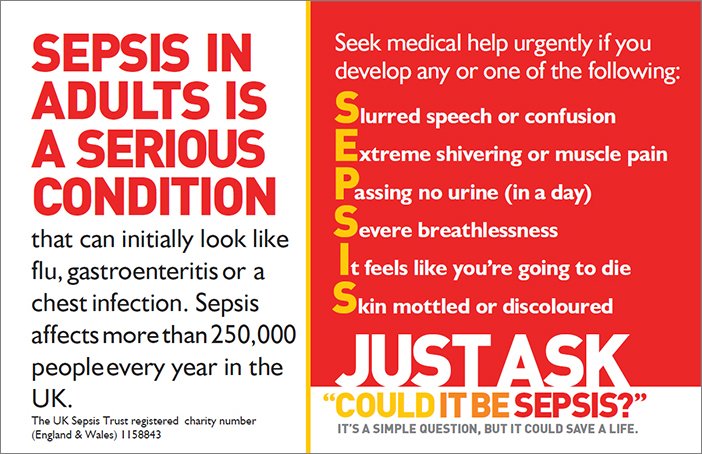
Recognising the Symptoms: The symptoms of Sepsis can be remembered with the acronym 'SEPSIS':
- S: Slurred speech or confusion
- E: Extreme shivering or muscle pain
- P: Passing no urine (in a day)
- S: Severe breathlessness
- I: It feels like you're going to die
- S: Skin mottled or discoloured
If you or someone else is experiencing any of these symptoms, seeking medical attention is crucial.
Early Intervention is Key
Early recognition and treatment of Sepsis can significantly improve the chances of recovery. If you suspect Sepsis, it's crucial to get to the nearest NHS hospital or contact your GP immediately. The NHS is equipped to provide rapid assessment and treatment for Sepsis, which may include antibiotics and other supportive measures.
Preventing Infections
Preventing infections can reduce the risk of developing Sepsis. Ensure to:
- Keep vaccinations up to date
- Practice good hygiene, like handwashing
- Seek prompt medical attention for infections
Sepsis is a medical emergency that requires immediate attention. Understanding the signs and seeking prompt medical care can significantly improve outcomes. The NHS provides comprehensive care for sepsis patients, and it's crucial to utilise these resources if you suspect you or a loved one may be suffering from Sepsis. Through awareness and education, especially on platforms like World Sepsis Day, we can work together to reduce the impact of Sepsis and save lives.
For more information on Sepsis, you can visit:
- This page provides a detailed overview of the symptoms of Sepsis and its life-threatening nature.
- Information about who is more likely to get Sepsis and how to avoid infections.
Signs of Sepsis and What to Do (PDF) - NHS England
- An easy-read document detailing the symptoms of Sepsis and the steps to take if you suspect Sepsis.
Treatment and Recovery from Sepsis - NHS
- NHS information about treatments and recovery from Sepsis, post-sepsis syndrome, and where to get support.
Our Work on Sepsis - NHS England
- Information on the clinical policy and work being done on Sepsis by NHS England.
Easy-Read Information: Sepsis - NHS England
- Easy-read documents providing information about how to avoid Sepsis, spotting the signs of Sepsis, and problems after Sepsis.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Martha's Rule: A Lifeline for Patients and Families in the NHS
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.22.1" _module_preset="default"][et_pb_row _builder_version="4.22.1" _module_preset="default" theme_builder_area="post_content"][et_pb_column _builder_version="4.22.1" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.22.1" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0"]
Martha's Rule is a proposed healthcare initiative in the United Kingdom that aims to empower patients and their families with the right to seek a second medical opinion. Named after Martha Mills, a 13-year-old girl who tragically died from preventable sepsis, the rule is gaining traction and support, including the Parliamentary and Health Service Ombudsman and Healthwatch. Here, we look at Martha's Rule's significance and potential impact on the NHS and patient care.
The Tragic Case of Martha Mills
Martha Mills was a 13-year-old girl enjoying a family holiday in Wales when she sustained a severe injury to her pancreas after falling from her bike. She was admitted to King's College Hospital in London, a specialist centre for children with pancreatic issues. Despite several opportunities to escalate her care, Martha's deteriorating condition was not adequately addressed. She developed sepsis and passed away, a tragedy that an inquest later ruled could have been prevented with better care.
What is Martha's Rule?
Martha's Rule aims to serve as an extra safeguard for patients or their loved ones who want a second opinion about treatment options, particularly when there is a suspected deterioration or serious concern. The rule would shift the balance of power from medical discretion to the patient or their family, enabling them to trigger a request for a second clinical opinion directly.
Support and Advocacy
Rob Behrens of the Parliamentary and Health Service Ombudsman has expressed full support for the introduction of Martha's Rule. He emphasised the need for patients to be listened to, citing numerous cases where patients were failed by their doctors due to a lack of attention. Healthwatch also backs the initiative, highlighting its potential to save lives if implemented correctly.
International Precedents
Similar systems exist globally, including a measure in Australia known as "Ryan's Rule," named after Ryan Saunders, who died from an undiagnosed streptococcal infection. The rule allows patients or their families to request a clinical review if their condition deteriorates.
Future Prospects
Health Secretary Steve Barclay has tasked officials with exploring the feasibility of implementing Martha's Rule in the UK. The rule could be a significant step forward in improving patient safety and ensuring that the voices of patients and their families are heard.
Martha's Rule has the potential to be a transformative addition to the UK's healthcare system, offering a lifeline to patients and families who feel their concerns are not being adequately addressed. As the NHS continues to evolve, implementing such a rule could be pivotal in ensuring that no more lives are lost due to medical oversight.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
NHS Complaint Procedures
[et_pb_section fb_built="1" _builder_version="4.22.1" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_row _builder_version="4.22.1" _module_preset="default" custom_margin="-37px|auto|-37px|auto|true|false" custom_padding="0px|0px|0px|7px|false|false" hover_enabled="0" global_colors_info="{}" theme_builder_area="post_content" sticky_enabled="0"][et_pb_column type="4_4" _builder_version="4.22.1" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_text _builder_version="4.22.1" _module_preset="default" custom_padding="|44px||||" hover_enabled="0" global_colors_info="{}" theme_builder_area="post_content" sticky_enabled="0"]
The NHS values feedback, both positive and negative, as it contributes to service improvement. If you are unhappy about the care, treatment, or service you've experienced from the NHS or a GP, you are entitled to make your voice heard. Your feedback could instigate changes that benefit both you and others in the future, and there are many reasons why it is important:
Accountability
Healthcare providers are responsible for delivering a high standard of care. When they fall short, they should be held accountable. Complaints can serve as a mechanism for this accountability.
Quality Improvement
Feedback is essential for any organisation that aims to improve. By pointing out what went wrong, you can help the NHS identify areas for improvement. This can lead to changes in procedures, training, and resource allocation, ultimately raising the quality of care for everyone.
Patient Safety
If you've experienced a lapse in the standard of care, others may have too. By bringing attention to the issue, you could be helping to prevent future mistakes that compromise patient safety.
Transparency
Hospitals and GP practices benefit from being transparent about their successes and failures. Complaints can be a form of data that helps the public and the organisation understand how well it is performing.
Empowerment
Making a complaint can be empowering for patients and families. It gives you a voice and can help you feel like an active participant in your healthcare rather than a passive recipient.
Legal and Ethical Reasons
In some cases, complaints may lead to legal action or disciplinary measures against healthcare providers who have been negligent or have violated professional standards.
Resource Allocation
Complaints can highlight areas where resources are lacking. This could lead to increased funding or other resources being allocated to address the issue.
Public Trust
Maintaining public trust is crucial for a publicly funded system like the NHS. Addressing complaints effectively is an integral part of maintaining this trust.
Understanding Your Rights
Before you proceed with a complaint, it's crucial to understand your rights as a patient. The NHS Constitution outlines these rights, which include:
- The right to high-quality care
- The right to be treated with dignity and respect
- The right to confidentiality
- The right to complain and have your complaint investigated
Initial Steps to Take
Identify the Issue
Before making a complaint, clearly identify the issue you're facing. Is it related to:
- Medical treatment?
- Staff attitude?
- Waiting times?
- Facilities?
Clearly understanding the issue will help you articulate your complaint more effectively.
Direct Communication with the Service Provider
If you're unhappy with an NHS service, it's often beneficial to discuss your concerns directly with the service, either with the clinician or the service manager. Many issues can be sorted out swiftly at this stage.
Patient Advice and Liaison Service (PALS)
Before moving on to formal complaints, you may want to speak to the Patient Advice and Liaison Service (PALS) who can:
•Help you with health-related questions
•Help resolve concerns or problems
•Tell you how to get more involved in your own healthcare
PALS can give you information about:
•The NHS
•The NHS complaints procedure
•Support groups outside the NHS
You can usually find a PALS office in NHS hospitals, or you can search for your nearest PALS online.
NHS Complaints Advocate
If you're contemplating making a formal complaint, you can seek assistance from an NHS complaints advocate. They can guide you in drafting a complaint letter and may accompany you to meetings. However, they cannot complain on your behalf.
Informal Complaints
Verbal Complaints
Sometimes, issues can be resolved quickly through informal channels. You can start by speaking directly to the clinician or a manager. This is often the quickest way to address minor concerns.
Written Complaints
If you're uncomfortable speaking directly or the issue is more serious, you can write an informal complaint via email or a letter. Make sure to include:
- Your name and contact details
- A clear description of the issue
- What you would like to happen as a result
Formal Complaints
Identifying the Appropriate Body
You can complain directly to the NHS service provider (such as a GP, dentist, or hospital) or to the commissioner of the services. If your complaint involves multiple organisations, you need only file one complaint, and the organisation that receives it will coordinate with the others.
Time Constraints
Complaints should ideally be made within 12 months of the incident or of becoming aware of the issue. This timeframe can be extended under specific conditions.
Methods of Filing a Complaint
Complaints can be lodged verbally, in writing, or via email. If you're filing a complaint on someone else's behalf, their written consent will be required.
What to Anticipate After Filing a Complaint
- Acknowledgement: You should anticipate an acknowledgement and an offer for a discussion regarding handling your complaint within three working days.
- Investigation: Your complaint will undergo an investigation, and you'll subsequently receive a written response outlining the findings, apologies if warranted, and actions taken as a result of your complaint.
- Ombudsman: If you're not content with the outcome, you can escalate your complaint to the Parliamentary and Health Service Ombudsman.
Alternative Avenues for Feedback
- Friends and Family Test (FFT): A quick and anonymous method for offering feedback.
- Patient Reported Outcome Measures (PROMs): Specifically for patients who have recently undergone hip or knee replacement surgery.
Your opinion matters. If you're dissatisfied with the healthcare services you've received, you have the right to file a complaint. However, it's worth noting that the way complaints are made and handled is also important. Complaints should be constructive, specific, and based on facts to be most effective. They should be made through the appropriate channels and following the procedures set out by the healthcare provider.
For more in-depth information, you can visit the NHS website.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Accessing GP Services: A Detailed Overview
[et_pb_section fb_built="1" _builder_version="4.22.1" _module_preset="default" global_colors_info="{}"][et_pb_row _builder_version="4.22.1" _module_preset="default" custom_margin="-37px|auto|-37px|auto|true|false" custom_padding="0px|0px|0px|19px|false|false" global_colors_info="{}"][et_pb_column type="4_4" _builder_version="4.22.1" _module_preset="default" global_colors_info="{}"][et_pb_text _builder_version="4.22.1" _module_preset="default" custom_padding="|44px||||" global_colors_info="{}"]
In May 2023, the UK government and NHS announced a multi-million-pound overhaul of primary care services to make it easier for patients to access their general practitioners (GPs). Here, we provide a detailed overview of what these changes mean for patients, from the technology upgrades to the role of care navigators.
Key Highlights of the New Plan
- Immediate Response to Patient Queries
Patients can now find out how their request will be handled on the same day they contact their GP practice. This eliminates the need for patients to call back later to find out the status of their query.
- Technology Upgrades
This year, a £240 million investment will be made to replace old analogue phone systems with modern digital telephony. This ensures that patients never encounter engaged tones when calling their GP practice.
- Online Tools
Easy-to-use online tools will be introduced to help patients get the care they need as soon as possible. These tools will be integrated with the clinical systems, allowing practice staff to identify patients and their information quickly.
- Urgent and Non-Urgent Appointments
If a patient's need is urgent, they will be assessed and given an appointment on the same day. For non-urgent cases, appointments should be offered within two weeks, or patients will be referred to NHS 111 or a local pharmacy.
- Role of Care Navigators
Receptionists will be trained to become expert 'care navigators' who gather information and direct patients to the most suitable healthcare professional. This aims to simplify and streamline the process for patients.
What This Means for Patients
- Easier Access to GPs
The new plan aims to end the 8 a.m. scramble for appointments by improving technology and reducing bureaucracy. Patients will find it easier to get through to their general practice team online or over the phone.
- Faster Response Times
Patients will know how their query will be managed on the same day they make contact. This is a significant improvement over the previous system, where patients often had to call back or wait for a response.
- More Convenient Options
The introduction of modern online booking and messaging systems will offer patients a convenient way to get the help they need, freeing up phone lines for those who prefer to call.
- Specialised Care
Care navigators will help assess, prioritise, and respond to patient needs. They will direct patients to other professionals within the general practice or other medical professionals, such as community pharmacists, who can best meet the needs of the patients.
The government's new plan to overhaul primary care services is a significant step towards modernising how patients contact their GP surgeries. With technology upgrades, specialised care navigators, and a commitment to faster response times, patients stand to benefit greatly from these changes. The aim is to make things more convenient for patients and make the workload more manageable for general practice teams, thereby improving the overall healthcare system.
The full plan can be accessed here.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Understanding a Fever
[et_pb_section fb_built="1" _builder_version="4.21.0" _module_preset="default" global_colors_info="{}"][et_pb_row _builder_version="4.21.0" _module_preset="default" global_colors_info="{}"][et_pb_column type="4_4" _builder_version="4.21.0" _module_preset="default" global_colors_info="{}"][et_pb_text _builder_version="4.21.0" _module_preset="default" global_colors_info="{}"]
A fever, also known as pyrexia, is a common symptom that can occur in various illnesses and conditions. But what exactly is a fever, and why do we get one? It's important to understand this symptom, as it's often a sign that our bodies are fighting an infection.
What is a Fever?
A fever is an increase in your body's normal temperature range, usually in response to an illness or infection. While the average body temperature is typically around 36.5 to 37.2 degrees Celsius, a fever is generally agreed upon in the medical field to be a body temperature of 38 degrees Celsius or above.
Why Do We Get a Fever?
Fever is not an illness in itself but rather a symptom, often indicative of an underlying condition. It's essentially a defence mechanism of our bodies. When bacteria or viruses invade our systems, our immune system responds by increasing our body temperature. This elevated temperature helps the body to kill off the invading organisms, as many of them cannot survive in higher temperatures.
Moreover, a fever also boosts the body's immune response by stimulating the production of white blood cells, the soldiers of our immune system, and other substances that help fight off infections.
What Constitutes a Fever?
While it's important to remember that everyone's 'normal' body temperature can vary slightly, the NHS categorises a fever in adults as a body temperature of 38 degrees Celsius or higher. However, even a slight elevation in temperature may cause discomfort and is usually the first sign of an illness. Please note it's not always easy to take a temperature accurately. If you feel hot or shivery, you may have a high temperature even if a thermometer says your temperature is below 38C.
Normal Temperature Limits
While the average body temperature for a healthy adult typically ranges between 36.5 and 37.2 degrees Celsius, it's normal for your body temperature to fluctuate throughout the day. For instance, it tends to be lower in the early morning and higher in the late afternoon and evening.
However, if your body temperature exceeds 38 degrees Celsius, it's usually a sign that your body is fighting an infection or illness. In the case of a very high fever of 39.5 degrees Celsius or higher, it's crucial to seek medical attention immediately, as this could indicate a severe infection.
Why Do We Shake During a Fever?
Fever often comes with chills or shivering, which can seem paradoxical when your body is overheated. This shaking is essentially a side effect of your body trying to increase its temperature. The process is triggered by the hypothalamus, our body's thermostat, which instructs our muscles to contract and relax rapidly to generate warmth, leading to what we recognise as shivering.
So, while fevers can be uncomfortable, they are often a sign that your body is doing exactly what it needs to do to fight off an infection or illness. However, it's important to monitor a fever closely and seek medical help if the fever is high, persistent, or accompanied by other severe symptoms such as confusion, difficulty breathing, or severe pain.
You can read more on the NHS.uk website here.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Living with & Managing Chronic Illness
[et_pb_section fb_built="1" theme_builder_area="post_content" _builder_version="4.21.0" _module_preset="default" hover_enabled="0" sticky_enabled="0"][et_pb_row _builder_version="4.21.0" _module_preset="default" theme_builder_area="post_content"][et_pb_column _builder_version="4.21.0" _module_preset="default" type="4_4" theme_builder_area="post_content"][et_pb_text _builder_version="4.21.0" _module_preset="default" theme_builder_area="post_content" hover_enabled="0" sticky_enabled="0"]
As many of you know, chronic conditions like Aspergillosis require more than just medical intervention. Chronic illnesses necessitate emotional resilience, adaptability, understanding, and physical strength. Patient-centric strategies have proven successful in managing illness and improving overall well-being and health outcomes, irrespective of the condition. The journey can be challenging, particularly when first diagnosed, but having an illness like Aspergillosis doesn't mean enduring a life of constant suffering.
What do we mean by manageable?
"Manageable" does not mean that your illness will completely disappear or you will no longer feel its effects. Instead, it means that the symptoms can be controlled to such an extent that they do not dominate your life or altogether remove your ability to function. Managing a chronic condition involves developing a comprehensive and tailored approach incorporating medication, lifestyle adjustments, emotional well-being, and social support.
Chronic conditions require more than medication
Understanding Your Illness
Knowledge is power. Understanding your illness, its symptoms, triggers, and progression will help you manage it more effectively. Ask your doctor(s) questions, do your own research, and consider joining support groups where you can learn from others' experiences.
Acknowledging limitations
When we discuss acknowledging limitations while living with Aspergillosis, there's a metaphor that captures this struggle: The Spoon Theory.
The Spoon Theory, conceived by Christine Miserandino, is a valuable metaphor within the chronic illness community to explain the energy required to live with such conditions. In this analogy, 'spoons' represent energy units. Each day, a person has a finite number of 'spoons' and must budget their activities to ensure they don't run out of 'spoons' before the day ends.
So, how does this relate to acknowledging limitations with Aspergillosis?
Physical Limitations
With Aspergillosis, common physical symptoms like fatigue or breathlessness may require more 'spoons' than usual. Understanding your body's signals and resting when necessary helps you conserve your 'spoons'.
Emotional Limitations
Chronic illness can be emotionally draining. It's normal to feel uncertain and anxious about your condition. According to the National Institute of Mental Health (NIMH), people with chronic illnesses may be more likely to suffer from depression. Therefore, depression is a common complication of chronic illness.
Managing feelings of anxiety or depression requires 'spoons'. Acknowledging your emotional health and seeking help and support when you need it can assist in managing your emotional energy better.
Social Limitations
Every social activity costs 'spoons'. While it's crucial to maintain a social life, it's equally important to recognise when you might need to prioritise rest and recovery.
Work Limitations
The energy expended at work needs to be factored into your 'spoon' budget. Sometimes, it may require a conversation with your employer to adjust your workload or responsibilities to accommodate your health needs.
Understanding and applying the Spoon Theory to your life can be a powerful tool in acknowledging and managing your limitations. It's not about resigning yourself to these limitations but prioritising and becoming effective at working around them.
Each of you will have a different number of 'spoons' each day, and what may cost one spoon for some may cost five for another. That's why it's so crucial to respect and acknowledge our boundaries.
The power of exercise
Exercise plays an integral role in maintaining our health and well-being. Regular physical activity can significantly improve quality of life, boost mood, enhance lung function, and strengthen the immune system. However, the thought of exercise might seem daunting given the physical constraints of Aspergillosis. But it's about finding what works best for you.
Exercise that suits your abilities
Remember, the objective is not to exhaust yourself but to gradually improve your endurance and strength within your limits. Lower-intensity activities such as walking, stretching exercises, or chair-based workouts can be beneficial starting points. Even small activities like light household chores can contribute to your daily exercise.
Pulmonary Rehabilitation
These are programmes specifically designed for people with lung conditions. They involve a combination of exercises to improve lung function, education, and emotional support. Trained healthcare professionals supervise these programmes to ensure safety and efficacy.
Breathing exercises
Exercises like pursed-lip or diaphragmatic breathing can improve lung capacity and help manage breathlessness, a common symptom in Aspergillosis.
Yoga and Meditation
Gentle yoga poses combined with mindful breathing can improve flexibility, balance, and strength while also helping with stress management.
Staying consistent
The key is regularity rather than intensity. Even 10-15 minutes of exercise daily can make a difference. As your endurance builds, you can gradually increase the duration and possibly the intensity of your workouts.
Work with professionals
Always consult your care team before starting a new exercise regimen. They can guide you.
Listen to your body
Most importantly, listen to your body. If you feel excessively tired or experience difficulty breathing, it's time to rest. Remember, acknowledging your limits is not a weakness; it's an essential part of managing your health.
Mental health matters
Living with a chronic illness like Aspergillosis can be physically challenging, but it also exacts a toll on our mental health. Anxiety, depression, stress, and feelings of isolation are not uncommon. Acknowledging these emotions and finding ways to manage them is as important as managing the physical symptoms of the illness.
Understanding the Impact
Chronic illnesses can lead to a range of emotional responses: fear about what the future holds, frustration over physical limitations, feelings of isolation due to changes in lifestyle or others' inability to fully understand your experience. Understanding that these are normal reactions to your situation is the first step towards addressing them.
Communication
One of the most powerful tools in managing mental health is open communication. This could be with family, friends, a support group, or a professional counsellor. Discussing your feelings can provide relief and offer new perspectives.
Professional Help
Psychologists, psychiatrists, and therapists can provide strategies to cope with the stress, anxiety, and depression that can accompany chronic illnesses. Cognitive-behavioural therapy, mindfulness-based stress reduction, and other techniques can help you navigate your emotional journey.
Peer Support
We talk about this a lot, and many of you reading this will already realise the benefits because you attend our weekly meetings. Connecting with others who are dealing with similar experiences can be incredibly helpful. Support groups provide a platform to share experiences, learn from others, and gain emotional comfort from knowing you're not alone.
Self-care
Prioritise activities that you enjoy and that help you relax. This could be reading, listening to music, gardening, or any hobby that provides a sense of calm. Mindfulness exercises, yoga, and meditation can also be effective in reducing stress and promoting mental well-being.
Depression is not a weakness
It's not just the physical discomfort and limitations that pose a challenge. Still, the emotional burden carried with a persistent health condition can also be substantial. Thus, depression is a common complication of chronic illness. Still, it doesn't have to be a normal part of chronic illness. Depression can manifest through persistent sadness, loss of interest in previously enjoyed activities, difficulty sleeping, or changes in appetite. It's important to recognise that depression is not a sign of weakness or a normal part of living with a chronic illness. It's a serious but treatable condition. If you or someone you care for shows signs of depression, seeking help from healthcare professionals is crucial. Therapies such as cognitive-behavioural therapy, medication, or a combination of both can effectively manage depression. Remember, taking care of your mental health is a critical part of managing a chronic illness.
Remember, it's okay to have tough days. Your illness does not define you, and it's okay to ask for help when needed. Celebrate your achievements, no matter how small, and focus on the strengths that help you navigate your challenges.
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
NAC CARES Team Joins European Lung Foundation (ELF) Patient Organisation Network
[et_pb_section fb_built="1" _builder_version="4.21.0" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_row _builder_version="4.21.0" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.21.0" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_image src="https://aspergillosis.org/wp-content/uploads/2023/06/IMG_9945.jpg" _builder_version="4.21.0" _module_preset="default" theme_builder_area="et_body_layout" title_text="IMG_9945" hover_enabled="0" sticky_enabled="0" align="center"][/et_pb_image][et_pb_text _builder_version="4.21.0" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"]
The National Aspergillosis CARES Team are excited to announce its membership in European Lung Foundation (ELF) Patient Organisation Network. This collaboration marks a milestone in the team's commitment to enhancing the lives of individuals affected by aspergillosis.
Founded in 2000 and working in partnership with the European Respiratory Society (ERS), ELF is a patient-led organisation that works internationally to bring patients and the public together with healthcare professionals to improve lung health and advance diagnosis, treatment, and care.
The ELF Patient Organisation Network is a hub for respiratory patient organisations throughout Europe, fostering knowledge exchange, collaboration, and advocacy initiatives to improve respiratory health and well-being across the continent. Membership of the network provides the CARES Team with access to invaluable resources, expertise, and opportunities to positively impact the lives of those living with aspergillosis.
As an active participant in this network, the NAC CARES Team will contribute expertise, raise awareness at both national and European levels, and help drive positive change. In addition to knowledge sharing and advocacy, the ELF Patient Organisation Network offers opportunities for networking and collaboration. By connecting with like-minded organisations, the team can establish partnerships, share experiences, and collaborate on joint initiatives to create a more supportive environment for individuals living with aspergillosis in Europe.
You can read more about ELF here: https://europeanlung.org/en/
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
