Secondary Adrenal Insufficiency
[et_pb_section fb_built="1" _builder_version="4.16" global_colors_info="{}" theme_builder_area="post_content"][et_pb_row _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.16" custom_padding="|||" global_colors_info="{}" custom_padding__hover="|||" theme_builder_area="post_content"][et_pb_text _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content"]
This month's (March) patient meeting included a presentation by Endocrinology Specialist Nurses from Manchester Royal Infirmary. This was a talk we requested as we know secondary adrenal insufficiency is a concern for many patients.
Allergic bronchopulmonary aspergillosis (ABPA) is a complex respiratory condition that occurs when the immune system overreacts to the Aspergillus fungus, leading to inflammation and potential lung damage. To manage the symptoms of ABPA, patients are often prescribed corticosteroid medications. However, long-term use of these medications can lead to a condition called secondary adrenal insufficiency. Watch the talk below to learn more about the condition, it's diagnosis, management and treatment.
[/et_pb_text][et_pb_video src="https://youtu.be/W6RLUeOjUrw" _builder_version="4.20.2" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][/et_pb_video][/et_pb_column][/et_pb_row][/et_pb_section]
Virtual Support Meetings Moving from Zoom to Microsoft Teams
[et_pb_section fb_built="1" _builder_version="4.20.2" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_row _builder_version="4.20.2" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.20.2" _module_preset="default" global_colors_info="{}" theme_builder_area="post_content"][et_pb_text _builder_version="4.20.2" _module_preset="default" hover_enabled="0" global_colors_info="{}" theme_builder_area="post_content" sticky_enabled="0"]
We will, in the coming weeks, be moving our virtual patient support meetings from the Zoom platform to Microsoft Teams. The NAC Cares Team understands that for some, this is an unfamiliar application, and the change can be daunting. We will be assisting in this transition and helping guide people by utilising both platforms.
Microsoft Teams is a powerful tool that offers all the same features as Zoom. Here's a step-by-step guide on how to attend the meeting as a guest:
The meeting link works in a similar way to Zoom, and you can register for a link through Eventbrite. If you have any issues, you can contact the CARES Team at nac.cares@mft.nhs.uk
Clinking the link will open a web page, where you'll see two choices: Download the Windows app and Join on the web instead. If you join on the web, we advise the use of Google Chrome. Your browser may ask if it's okay for Teams to use your mic and camera. Be sure to allow it so you'll be seen and heard in your meeting.
If you want to install Microsoft Teams on your device, you can follow the prompts and on-screen instructions. Once the app is installed, enter your name and choose your audio and video settings and then hit join now.
If you enter the meeting lobby, wait for one of the CARES Team to admit you.
During the meeting:
- Once you've joined the meeting, you'll be able to see and hear the other patients/relatives.
- You can choose to turn on or off your camera and microphone by selecting the camera or microphone icons at the bottom of the screen.
- There is a chat function to send messages to other participants.
Leaving the meeting:
To leave the meeting, select the "Leave" button at the top-right corner of the screen.
If you wish to download Microsoft Teams you can do so via the link below:
https://www.microsoft.com/en-us/microsoft-teams/download-app
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
IgG and IgE explained
[et_pb_row][et_pb_column type="4_4"][et_pb_text]
Immunoglobulins, also known as antibodies, are proteins produced by the immune system in response to the presence of foreign substances, such as viruses and bacteria. There are different types of immunoglobulins, including IgG and IgE, which play different roles in the immune system. In aspergillosis, both IgG and IgE antibodies play important roles in the immune response to the Aspergillus fungus. This post aims to provide important information about the differences between IgG and IgE.
What is IgG?
IgG is the most common type of immunoglobulin in the bloodstream, accounting for about 75% of all antibodies in the body. IgG plays an important role in fighting off bacterial and viral infections and is also involved in the immune response to certain types of cancer cells. IgG can cross the placenta and provide protection to a developing foetus, which is why it is referred to as a "maternal antibody."
Elevated levels of IgG antibodies to Aspergillus are often seen in individuals with Chronic Pulmonary Aspergillosis (CPA), and measuring IgG antibody levels is an important diagnostic tool for the condition.
What is IgE?
IgE is a type of immunoglobulin that plays a role in the allergic response. IgE is produced in response to exposure to allergens, such as pollen, pet hair, and certain food, and for patients with allergic bronchopulmonary aspergillosis - aspergillus fungus. When IgE binds to an allergen, it triggers the release of histamine and other chemicals, leading to the symptoms of an allergic reaction, such as:
- Wheezing
- Coughing
- Shortness of breath
- Chest pain or tightness
Differences between IgG and IgE
There are several differences between IgG and IgE, including:
- IgG plays a role in fighting off bacterial and viral infections, while IgE is involved in the allergic response.
- IgG has a longer half-life in the bloodstream than IgE, which means it stays in the body longer.
- IgG takes longer to produce in response to an infection or exposure to an antigen, while IgE is produced rapidly in response to an allergen.
Both IgG and IgE antibodies play important roles in the immune response in aspergillosis. While IgG helps to neutralise and eliminate the fungus, IgE triggers the allergic response and leads to symptoms in individuals with Allergic Bronchopulmonary Aspergillosis (ABPA). Measuring antibody levels to Aspergillus can be helpful in diagnosing and monitoring these conditions.
More information on the role of IgE and IgG can be found via the links below:
https://onlinelibrary.wiley.com/doi/10.1111/all.14908
https://www.britannica.com/science/immune-system/Classes-of-immunoglobulins
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
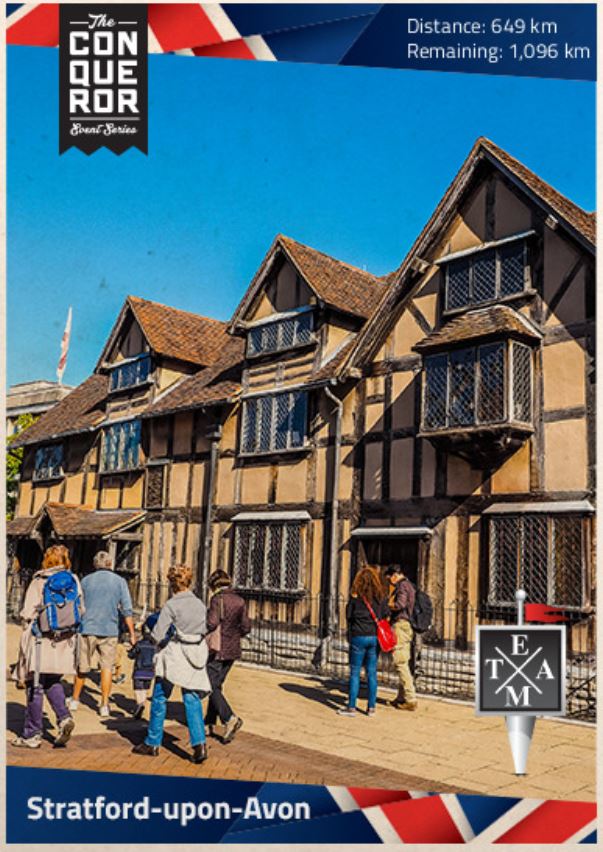
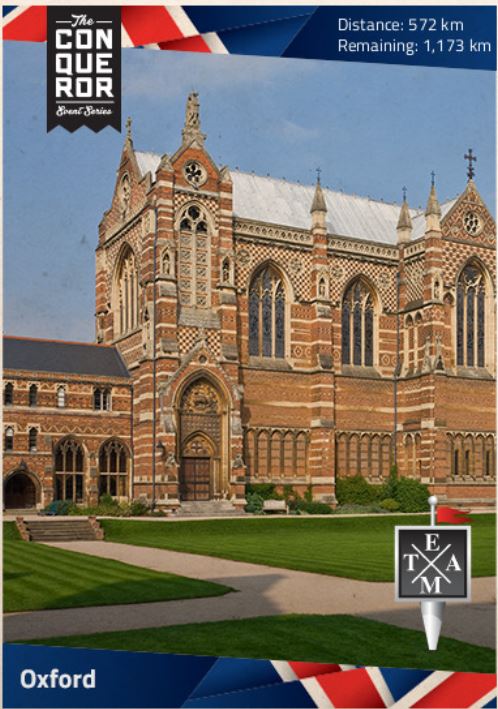
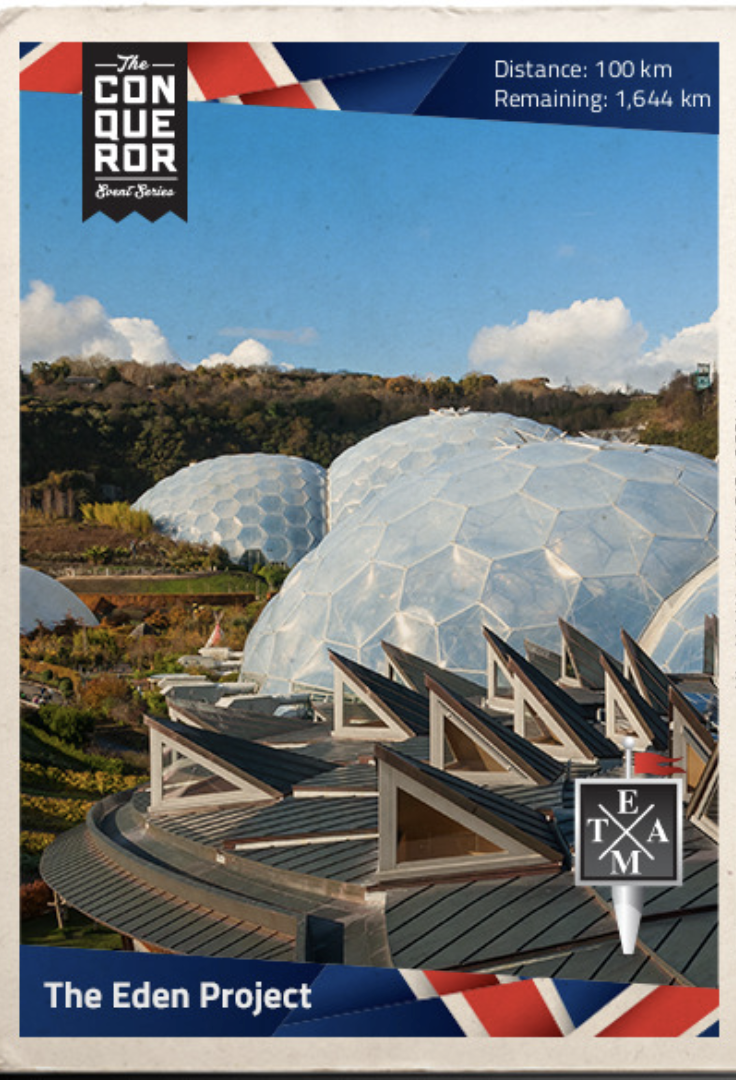
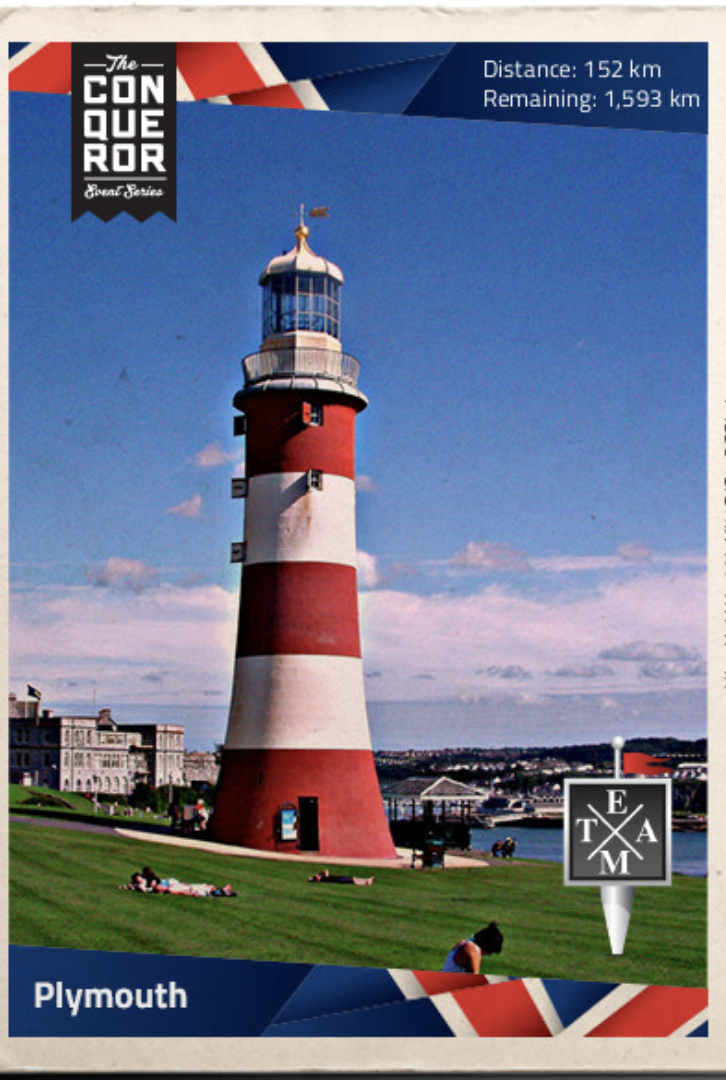
NAC CARES Virtual Challenge - 418.5 miles (673.54km down)
The NAC CARES Team are 30 days into their 100-day challenge to travel the length of the UK from Land End to John O' Groats (LEJOG). The last 30 days have seen the team run, cycle and walk to rack up the miles for the 1,084 mile (1,743km) challenge.
The team is outside Coventry and virtually passed through many well-known landmarks, including Stratford-Upon-Avon, The Royal Shakespeare Company Theatre, Oxford and Kenilworth Castle. The beauty of a virtual challenge is that even with the impending cold weather forecast, the team can still check off the miles on treadmills and indoor bikes so, in the words of a Disney Princess, let it snow!
The work of the Fungal Infection Trust (FIT) improves awareness, treatment and outcomes for all those affected by fungal disease. FIT is a small charity who have, over the years, supported the work of the NAC CARES Team, allowing them to maintain their unique work. Every pound raised will help the Trust continue to help people around the world. You can read more about their work here.
To donate, visit here.



Accessing GP services
Changes to GP contracts for 2023/2024 mean patients should be able to access appointments without enduring the 8am scramble and subsequent telephone queue we are all so very used to.
The new GP contract was published on Monday, 6 March by NHS England and will be in place from next month. The change is part of NHS England's goal to ensure equitable and consistent patient access. The contract states that:
'Patients should be offered an assessment of need, or signposted to an appropriate service, at first contact with the practice. Practices will therefore no longer be able to request that patients contact the practice at a later time.'
While the contract's wording does not elaborate on an appropriate service, this will likely mean telephone and in-person appointments, referral to pharmacists for minor illnesses, physiotherapists for muscular skeletal issues, or Accident and Emergency Departments for more urgent health concerns.
The contract change will ensure patients can access timely and appropriate care, but it will no doubt take time for practices to implement the changes.
NAC CARES Virtual Challenge - Week 2
The NAC CARES Team are seventeen days into their virtual Lands End To John O'Groats (LEJOG) challenge, and this last week has seen them cover a further 65.86 miles (106.1km). This means the team have covered a total of 227.29 miles (365.80km), equating to 1/5 of the total distance.
This week's miles were dedicated to aspergillosis patient Ian Stratton, an avid runner with Brackla Harriers who recently passed away.
This week's collective effort has again been achieved with team walks, trail, road and treadmill running, and more long hours on static bikes. This week's virtual landmark was the stunning Durdle Door, a natural limestone arch on the Jurassic Coast near Lulworth in Dorset, England.
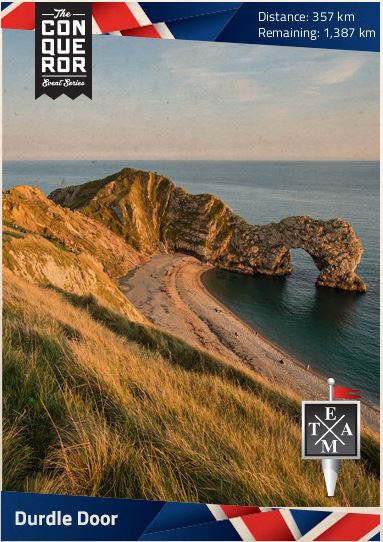
The virtual challenge, which the team began on World Aspergillosis Day 2023 (February 1st), covers the length of the UK and will see the team run, cycle and walk a total of 1,084 miles (1,743km).
The goal is to complete the distance in 100 days and to raise just £1 for every km travelled.
If you would like to read more about the Fungal Infection Trust (FIT), which the team are fundraising for, and donate, then follow the link https://www.justgiving.com/campaign/LEJOG-for-Aspergillosis
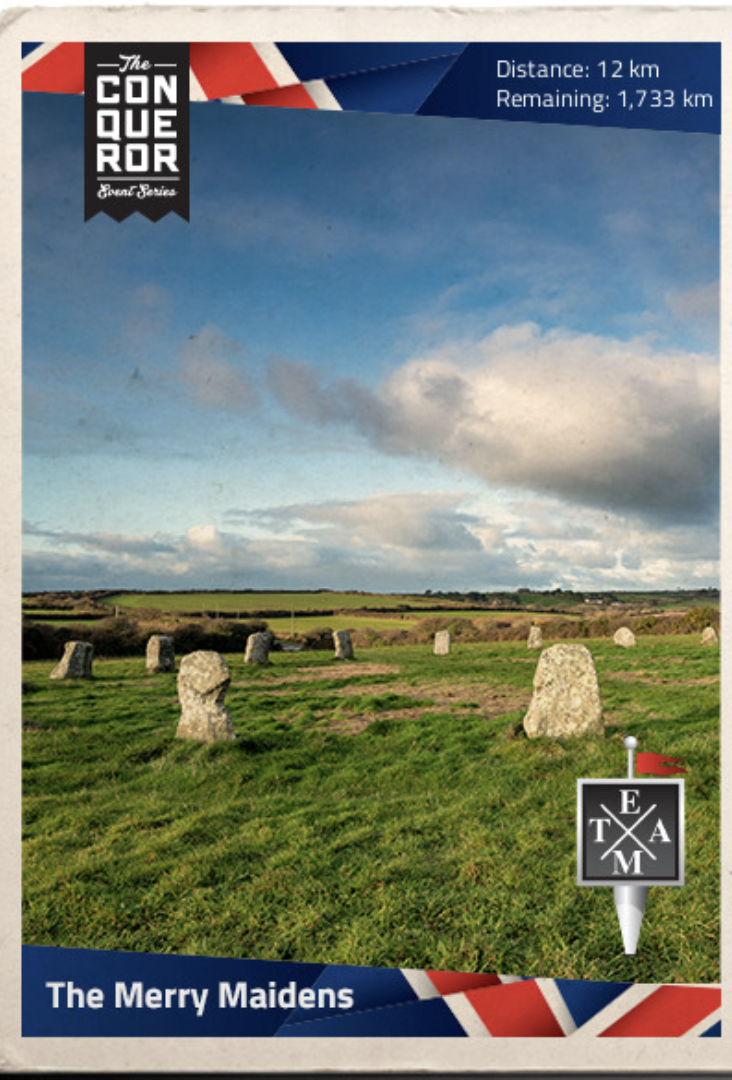
NAC CARES Virtual Challenge - Week 1
[et_pb_section admin_label="section"]
[et_pb_row admin_label="row"]
[et_pb_column type="4_4"][et_pb_text admin_label="Text"]
It has been ten days since the NAC CARES Team embarked on their virtual Lands End To John O'Groats (LEJOG) challenge. The virtual challenge, which the team began on World Aspergillosis Day 2023 (February 1st), covers the length of the UK and will see the team run, cycle and walk a total of 1,084 miles (1,743km).
The goal is to complete the distance in 100 days and to raise just £1 for every km travelled.
The first ten days have already seen the team cover 14% of the distance; that is 161.4 miles (259.70km), and they are ahead of schedule by a whopping 68.48 miles (110.2km)! The collective effort has been achieved with walks, running, and long hours on static bikes and treadmills. Check out some of the areas we have passed below, and let us know if you live nearby!
The team will be dedicating the next week of miles and km to aspergillosis patient Ian Stratton, an avid runner with Brackla Harriers who recently passed away.
If you would like to read more about the Fungal Infection Trust (FIT) which the team are fundraising for, and donate, then follow the link https://www.justgiving.com/campaign/LEJOG-for-Aspergillosis


[/et_pb_text][/et_pb_column]
[/et_pb_row]
[/et_pb_section]
The importance of detecting cancer early
[et_pb_section fb_built="1" admin_label="section" _builder_version="4.18.0" custom_padding="5px||5px|||" global_colors_info="{}" theme_builder_area="post_content"][et_pb_row admin_label="row" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" custom_margin="|-33px||21px||" custom_padding="5px|0px||||" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.16" custom_padding="|||" global_colors_info="{}" custom_padding__hover="|||" theme_builder_area="post_content"][et_pb_text admin_label="Text" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" custom_margin="-41px|-146px||||" global_colors_info="{}" theme_builder_area="post_content"]
Our focus at the National Aspergillosis Centre is to raise awareness and support those with aspergillosis. Still, it is vital as an NHS organisation that we raise awareness of other conditions because, sadly, a diagnosis of aspergillosis does not make you impervious to everything else, and a chronic illness has the potential to mask the symptoms of other conditions like cancer.
The ever-growing pressure on the NHS, increased waiting times, a growing reluctance amongst many to seek medical attention, and a lack of understanding of the common symptoms of many cancers are all factors that can lead to an extended diagnostic interval, which in turn reduces treatment options. Therefore, earlier recognition of symptoms by patients is crucial in mitigating other factors that delay diagnosis.
It is important to note that not all alarm symptoms are cancer. Still, cancer incidence and mortality projections estimate that 1 in 2 people in the UK will be diagnosed with cancer in their lifetime(1), so last week at our monthly patient meeting, we talked about cancer and the most common symptoms. Inspired by the incredible work of the late Dame Deborah James on raising awareness and breaking down the taboo attached to bowel cancer, we have compiled the content from that talk into one article.
What is Cancer?
Cancer starts in our cells.
Usually, we have just the right number of each type of cell. This is because cells produce signals to control how much and how often the cells divide.
If any of these signals are faulty or missing, cells might start to grow and multiply too much and form a lump called a tumour.
Cancer Research UK, 2022
Cancer Statistics
- Every two minutes, someone in the UK is diagnosed with cancer.
- Breast, prostate, lung and bowel cancers together accounted for over half (53%) of all new cancer cases in the UK in 2016-2018.
- Half (50%) of people diagnosed with cancer in England and Wales survive their disease for ten years or more (2010-11).
- Cancer is the cause of 27-28% of all deaths in England in a typical year.
Experts believe abdominal cancers - throat, stomach, bowel, pancreatic, ovarian - and urological cancers - prostate, kidney and bladder - are the most likely to go unrecognised.

The above chart shows cancer diagnoses by stage for some cancers in 2019 (the most current data). The stage of cancer relates to the size of the tumour and how far it has spread. Diagnosis at a later stage is related to lower survival.
Breast Cancer - Symptoms
- A lump or thickening in the breast which is different to the rest of the breast tissue
- Continuous breast pain in one part of the breast or armpit
- One breast becomes larger or lower/higher than the other breast
- Changes to the nipple - turning inward or changes shape or position
- Puckering or dimpling to the breast
- Swelling under the armpit or around the collarbone
- A rash on or around the nipple
- Discharge from one or both nipples
For more information visit:
https://www.breastcanceruk.org.uk/
https://www.cancerresearchuk.org/about-cancer/breast-cancer
Kidney Cancer - Symptoms
- Blood in the urine
- Low back pain on one side not through injury
- A lump on the side or lower back
- Fatigue
- Loss of appetite
- Unexplained weight loss
- Fever that is not caused by an infection and that doesn't go away
For more information visit:
https://www.nhs.uk/conditions/kidney-cancer/symptoms/
https://www.cancerresearchuk.org/about-cancer/kidney-cancer/symptoms
Lung cancer
The symptoms of lung cancer can be particularly hard to differentiate for patients with aspergillosis. It is important to report any new symptoms, such as a change to a long-term cough, weight loss and chest pain to your GP or specialist consultant.
Symptoms
- A persistent cough that doesn't go away after 2/3 weeks
- A change in your long-term cough
- Increased and persistent breathlessness
- Coughing up blood
- An ache or pain in the chest or shoulder
- Repeated or persistent chest infection
- Loss of appetite
- Fatigue
- Weight loss
- Hoarsness
For more information visit:
https://www.nhs.uk/conditions/lung-cancer
https://www.cancerresearchuk.org/about-cancer/lung-cancer
Ovarian Cancer - Symptoms
- Persistent bloating
- Feeling full quickly
- Loss of appetite
- Changes in bowel habits
- Unexplained weight loss
- Pelvic or abdominal pain
- Needing to wee more frequently
- Fatigue
For more information visit:
https://www.nhs.uk/conditions/ovarian-cancer/
Pancreatic Cancer
Some of the symptoms of pancreatic cancer can closely resemble those of bowel conditions such as irritable bowel. See your GP if your symptoms change, get worse, or do not feel normal for you.
Symptoms
- Yellowing to the whites of your eyes or skin (jaundice)
- Itchy skin, darker pee and paler poo than usual
- Loss of appetite
- Fatigue
- Fever
Other symptoms can affect your digestion, such as:
- Nausea and vomiting
- Changes in bowel habits
- Stomach and/or back pain
- Indigestion
- Bloating
For more information visit:
https://www.nhs.uk/conditions/pancreatic-cancer
https://www.cancerresearchuk.org/about-cancer/pancreatic-cancer
https://www.pancreaticcancer.org.uk/
Prostate Cancer - Symptoms
- Urinating more frequently, often during the night (nocturia)
- Increased urgency to urinate
- Urine hesitancy (difficulty starting to urinate)
- Difficulty in passing urine
- Weak flow
- Feeling that your bladder has not emptied fully
- Blood in urine or semen
For more information visit:
https://www.nhs.uk/conditions/prostate-cancer
https://www.cancerresearchuk.org/about-cancer/prostate-cancer
Skin Cancer
Patients who are on antifungal medication are at an increased risk of developing skin cancer, therefore it is important to understand the symptoms and take adequate precautions with sun exposure to reduce the risk.
Symptoms
There are three main types of skin cancer:
- Malignant Melanoma
- Basal Cell Carcinoma (BCC)
- Squamous Cell Carcinoma (SCC)
Broadly, the signs are (shown in the image below):
BCC
- Flat, raised or dome-shaped spot
- Pearly or skin-coloured
SCC
- Raised, crusty or scaly
- Sometimes ulcerated
Melanoma
- An abnormal mole that is asymmetrical, irregular and has multiple colours

For more information visit:
https://www.cancerresearchuk.org/about-cancer/skin-cancer
https://www.nhs.uk/conditions/melanoma-skin-cancer/
https://www.nhs.uk/conditions/non-melanoma-skin-cancer/
Throat Cancer
Throat cancer is a general term that means cancer that starts in the throat, however, Doctors don't generally use it. This is because there are different types of cancer which can affect the area of the throat.
More information can be found here: https://www.macmillan.org.uk/cancer-information-and-support/head-and-neck-cancer/throat-cancer
General symptoms
- Sore throat
- Ear pain
- Lump in the neck
- Difficulty swallowing
- Change in your voice
- Unexplained weight loss
- A cough
- Shortness of breath
- A feeling of something stuck in the throat
For more information visit:
https://www.nhs.uk/conditions/head-and-neck-cancer/
Bladder Cancer - Symptoms
- Increased urination
- Urgency to urinate
- A burning sensation when passing urine
- Pelvic pain
- Flank pain
- Abdominal pain
- Unexplained weight loss
- Leg swelling
For more information visit:
https://www.nhs.uk/conditions/bladder-cancer/
https://www.cancerresearchuk.org/about-cancer/bladder-cancer
Bowel Cancer - Symptoms
- Bleeding from the bottom and/or blood in poo
- A persistent and unexplained change in bowel habit
- Unexplained weight loss
- Fatigue
- A pain or lump in the stomach
For more information visit:
https://www.bowelcanceruk.org.uk/about-bowel-cancer/
https://www.cancerresearchuk.org/about-cancer/bowel-cancer
(1)Smittenaar CR, Petersen KA, Stewart K, Moitt N. Cancer incidence and mortality projections in the UK until 2035. Br J Cancer 2016 Oct 25;115(9):1147-1155
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Drug Induced Photosensitivity
What is drug-induced photosensitivity?
Photosensitivity is the abnormal or heightened reaction of the skin when exposed to ultraviolet (UV) radiation from the sun. This leads to skin that has been exposed to the sun without protection becoming burnt, and in turn, this can increase the risk of developing skin cancer.
There are several medical conditions like lupus, psoriasis and rosacea that can increase a person's sensitivity to ultraviolet light. A more comprehensive list of known conditions can be found here.
Drug-induced photosensitivity is the most common type of skin-related adverse drug reaction and can occur as a result of topical and oral medications. Reactions happen when a component of the medication combines with UV radiation during sun exposure, causing a phototoxic reaction that appears as severe sunburn, identified by swelling, itchiness, profuse redness and in the worst cases, blistering and oozing.
Patients taking antifungal medications, in particular, Voriconazole and Itraconazole (the former being more widely known for causing reactions), are often aware of the increased risks of photosensitivity; however, these are not the only drugs that can induce an abnormal response to UV exposure. Other drugs that have been reported to cause photosensitivity are:
- NSAIDs (Ibuprofen (oral and topical), naproxen, aspirin)
- Cardiovascular medication (furosemide, ramipril, amlodipine, nifedipine, amiodarone, clopidogrel – just a few)
- Statins (simvastatin)
- Psychotropic drugs (olanzapine, clozapine, fluoxetine, citalopram, sertraline – just a few)
- Antibacterial medications (ciprofloxacin, tetracycline, doxycycline)
It is essential to note that the above list is not exhaustive, and reported reactions range from rare to frequent. If you think a medication other than your antifungal is causing a reaction to the sun, speak to your pharmacist or GP.
How to protect yourself
In most cases, patients can't stop taking the medication that can predispose them to photosensitivity. Staying out of the sun isn't always possible either - quality of life is always an important consideration; therefore, extra care should be taken to protect their skin while outside.
There are two types of protection:
- Chemical
- Physical
Chemical protection is in the form of sunscreen and sunblock. However, it is important to remember that sunscreen and sunblock are not the same. Sunscreen is the most common type of sun protection, and it works by filtering the sun's UV rays, but some still get through. Sunblock reflects the rays away from the skin and prevents them from penetrating it. When buying sunscreen, look for a sun protection factor (SPF) of 30 or above to protect against UVB and at least a UVA protection rating of 4 stars.
Physical protection
- NHS guidance advises staying in the shade when the sun is strongest, which in the UK is between 11am and 3pm from March to October
- Use a sunshade or umbrella
- A wide-brimmed hat that shades the face, neck and ears
- Long-sleeved tops, trousers and skirts made of close-weave fabrics that stop sunlight from penetrating
- Sunglasses with wraparound lenses and wide arms that conform to the British Standard
- UV protective clothing
Links to further information
Medical Alert Paraphernalia
[et_pb_section fb_built="1" admin_label="section" _builder_version="4.16" global_colors_info="{}" theme_builder_area="post_content" custom_padding="2px||2px||true|false"][et_pb_row admin_label="row" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content"][et_pb_column type="4_4" _builder_version="4.16" custom_padding="|||" global_colors_info="{}" custom_padding__hover="|||" theme_builder_area="post_content"][et_pb_text admin_label="Text" _builder_version="4.16" background_size="initial" background_position="top_left" background_repeat="repeat" global_colors_info="{}" theme_builder_area="post_content"]Medical identification items such as bracelets are designed to inform healthcare professionals of conditions that may impact treatment in an emergency where you cannot speak for yourself.
If you have a chronic condition, food or drug allergies, or take medications such as long-term steroids or anticoagulants, they may alter the treatment you might receive, and it is imperative that healthcare professionals know and can act accordingly. In a situation where you may be unconscious or unable to speak, a medical alert can provide vital information regarding conditions, medications and next-of-kin.
What medical alert items are available?
Many different medical alert items are available, the most common being a bracelet that is worn and easily identified in an emergency.
There are a number of reputable online companies where you can purchase a medical alert bracelet, a couple of which are listed below. Please ensure when purchasing online that the company is legitimate and that their jewellery will be recognised by the healthcare professionals.
https://www.medicalert.org.uk/collections/
https://www.amazon.co.uk/Medic-Alert-Bracelets/s?k=Medic+Alert+Bracelets
Lions Club Message in a Bottle
Lions Clubs Message in a Bottle is a simple but effective way for people to keep their basic personal and medical details where they can be found in an emergency on a standard form and in a common location – the fridge.
Message in a Bottle (known within Lions as MIAB) helps emergency services personnel to save valuable time in identifying an individual very quickly and knowing if they have any allergies or take special medication.
Paramedics, police, firefighters and social services support this Lions life-saving initiative and know to look in the fridge when they see the Message in Bottle stickers supplied. The initiative provides peace of mind that prompt and appropriate medical assistance can be provided, and next of kin/emergency contacts can be notified.
How to obtain a Message in a Bottle
Members of the public and other organisations can obtain a Message in a Bottle kit by contacting their local Lions club; more details are available here.[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
